Patient-Centered Payment for Primary Care
The Services Delivered by Primary Care Practices
High-quality primary care is an essential component of a high-value healthcare system.1 However, designing a payment system that successfully supports high-quality primary care is challenging because “primary care” is not one service but several different services. Since patients have different needs and different preferences for how their needs should be addressed, each patient will need and want to receive different types and numbers of these primary care services. As a result, “high quality primary care” will mean different things to different patients.
Primary care practices deliver three basic types of services2:
Wellness Care. Primary care practices help patients stay healthy by educating them about what they should do to maintain and improve their health and by ensuring that patients have obtained appropriate preventive care services, such as vaccinations and cancer screenings.
Chronic Condition Management. For patients who have one or more chronic diseases or long-term health problems, primary care practices not only prescribe appropriate treatments but also help patients understand how best to manage their condition(s) in a way that minimizes the number and severity of complications and slows the progression of the disease.
Non-Emergency Acute Care. For patients who experience a new symptom or have an injury that does not require emergency care, the primary care practice can either diagnose and treat the problem or arrange for appropriate testing and treatment from other healthcare providers.
There are some fundamental differences in the ways primary care practices need to deliver the services in these categories:
Acute care is inherently a reactive service – a patient only receives the service if they have an injury or experience a new symptom. Even if the problem is not an emergency, diagnosis and treatment should occur as soon as possible to prevent more serious problems from occurring and to minimize time away from work, school, etc.
In contrast, wellness care and chronic condition management should be primarily proactive, i.e., the goal should be to prevent health problems and chronic disease exacerbations before they occur, and to identify new health problems and treat them in early stages, rather than only taking action after a problem occurs or when the patient experiences an unrelated acute event.
In order to be effective, proactive and reactive services must be organized differently, and they must be customized appropriately to patients’ specific needs. Different skills and staff are needed to deliver the services in each category in the most efficient and effective way. As a result, the costs incurred by a primary care practice will depend on the number of patients who receive each type of service.
In addition, although all primary care practices deliver a basic level of services in each of the three categories, practices vary in terms of the scope of the services they offer. For example:
some primary care practices perform basic laboratory testing in the office, but others do not, and some perform more types of procedures (e.g., minor surgery or treatments for specific health conditions) than others. This depends on a variety of factors, including the availability of other providers in the community and the adequacy of payments.
some primary care practices also deliver services such as maternity care and psychological counseling, particularly in rural areas where there are no specialty medicine practices that deliver those services.
Not every patient will need these additional services, so different patients will be affected differently by whether a practice offers them; conversely, a practice’s ability to offer the services will depend on how many patients are likely to use them.
The Problems with Fee-for-Service Payment
Most primary care practices are paid on a fee-for-service basis, i.e., when the practice delivers a specific service to a patient, the practice receives a pre-defined fee associated with that service from the patient or their insurance plan.
In principle, fee-for-service payment can be very patient-centered, since the amount of payment the primary care practice receives will be customized to the specific types of services patients actually receive. Unfortunately, because of two problems in the way Medicare and health insurance plans have implemented fee-for-service payments for primary care, most primary care practices lose money when they deliver appropriate, high-quality primary care services:
There are no fees at all for many important primary care services, particularly services needed for proactive care. Traditionally, fees have only been paid for face-to-face office visits with physicians, nurse practitioners, or physician assistants and for procedures or tests; there has been little or no payment for phone calls and emails with patients or for education and assistance delivered by nurses and other practice staff to provide proactive care management.
The fee amounts are less than what it costs to deliver high-quality care. Primary care practices have generally been forced to spend less time with patients than is necessary or desirable because the fees paid per visit are too low to allow longer visits. Moreover, because the practice has to fill its schedule with patients each day in order to receive enough revenue to cover its costs, patients have difficulty obtaining an appointment or contacting their regular physician.
There are two additional problems with standard fee-for-service payment systems that can harm the quality of care for patients as well as cause financial problems for the primary care practice:
There is no assurance of the appropriateness or quality of the service that is delivered. Under fee-for-service payment, the primary care practice is paid for delivering a service to a patient even if the service was unnecessary, and the fee is the same regardless of the quality vof the service.
The primary care practice is penalized financially when patients are healthy. Because most fees are paid for treating and diagnosing health problems, if the primary care practice successfully helps a patient to stay healthy, it will receive fewer payments for that patient, and potentially no payments at all.
A truly patient-centered payment system must correct all of these problems in order for primary care practices to deliver high-quality care to all types of patients
Problems With Current and Proposed Payment Reforms
To date, three basic approaches have been used or proposed as alternatives to standard fee-for-service payments: (1) pay for performance and shared savings; (2) fees for additional services; and (3) population-based payment. As explained below, none of these approaches solves the problems in current fee-for-service systems3 or enables the delivery of patient-centered primary care.
Pay for Performance
Under this approach, a primary care practice can receive additional payments if it performs better than other practices on a set of payer-defined measures of quality, utilization, or spending, and its payments may be reduced if its performance is lower than what other practices achieve on these measures. This approach has been unsuccessful in improving either the quality or financial sustainability of primary care because it does not solve any of the problems with fee-for-service payment described above:
- There are no new fees for currently unpaid services. The primary care practice is still paid only for the same types of services that have been paid for in the past, and it loses money if it delivers care in different ways.
- Payments still fall short of the cost of quality care. Even if a practice qualifies for additional payments, the increase is typically too small to make up the shortfall between fee-for-service payments and the cost of delivering high-quality care. Moreover, the administrative burdens associated with quality measurement can cause the practice’s costs to increase more than the additional revenue it receives from performance-based payments.
- The measures used do not accurately or completely assess the quality of care delivered. Quality is assessed based on whether care for a patient met a general standard of quality, even if meeting the standard would have been undesirable or harmful for that particular patient. Moreover, because quality measures are only applicable to a narrow range of health conditions and services, there is no measure of quality at all for many types of health problems and patients.
- The primary care practice can be penalized if performance on a measure was poor due to factors outside of the practice’s control. For example, if a patient is unable to afford the services needed to achieve a good result on the quality measure (e.g., medications needed to treat diabetes), or if they are unwilling to use those services, the primary care practice will be scored as having failed on the measure for that patient and its payments may be reduced, even though the practice had no control over the factors affecting that patient’s adherence.
- There is no assurance of quality care for each patient. In addition, a primary care practice that scores well on a quality measure is still paid if it delivers poor-quality care for an individual patient. In fact, since performance-based payments are based on the percentage of all patients whose care met the quality standard, a practice may be paid more for delivering poor-quality care to an individual patient if the practice has higher-than-average quality scores for its other patients.
The most problematic versions of pay-for-performance are “shared savings” payment models that make additional payments to the primary care practice if the payer calculates that the total amount it spent on all of the healthcare services the patients received (including services from hospitals, specialists, etc.) was reduced or was lower than the amount it spent on similar patients who received care from other primary care practices. These payment models have all of the problems described above, plus a serious additional problem:
- The primary care practice can be paid more for withholding services the patient needs. Under a shared savings payment model, if a physician does not order a test, procedure, or medication for a patient, that is considered “savings,” regardless of whether the patient needed the service or not, and that physician can receive a portion of the savings. Similarly, if the physician orders a less expensive test, procedure, or medication than what is really required to address the patient’s health needs, that is also considered savings, and the physician practice may receive a financial bonus.
Fees for Additional Services
In recent years, Medicare and other payers have begun paying primary care practices for some additional types of services, including proactive services such as care management for patients with chronic conditions. Beginning in 2020, primary care practices could receive payments for delivering telehealth services to patients in their homes. However, these new payments have failed to fully address the problems in the current payment system:
- New payments are only for a subset of the services patients need. In general, new payments have only been made for narrowly-defined services and/or for specific types of patients. For example, Medicare’s Chronic Care Management payments are only for patients who have two or more chronic conditions, and the primary care practice can only receive the payment for a patient if the practice spends at least 20 minutes delivering services to the patient during the month. When Medicare began paying for telehealth services in 2020, the payments were initially paid only if there was a video connection with the patient, even if the patient did not have access to a computer or smartphone.
- Payment amounts do not cover the cost of delivering high-quality care. If a primary care practice needs to hire additional staff or incur other costs in order to deliver high quality care, it has to receive enough revenue to cover those costs. However, the amounts of additional payments are typically not based on any information about what it will actually cost to deliver the services, particularly in small practices.
- Restrictions intended to prevent inappropriate uses can prevent use of services when they are needed. Creating new fees for specific types of services creates fears that the services will be delivered when they are unnecessary or inappropriate. For example, the fees for telehealth visits that were authorized during the coronavirus pandemic enable a patient’s primary care physician to address certain types of patient needs and problems without requiring the patient to travel to the physician’s office. However, there are concerns that telehealth will be used when the patient could and should be seen in the office or when no visit at all is warranted. Proposed restrictions to prevent inappropriate uses could also prevent telehealth services from being used in appropriate situations.
Population-Based Payment
In a “population-based payment” system, a primary care practice receives a monthly payment for each patient instead of individual fees for office visits. (Some proposed payments would also replace fees for procedures and other services delivered by the primary care practice). The payments are referred to as “population-based” because the amount of payment depends on how many patients the practice treats, not how many services or what types of services the practices uses to treat them. Population-based payments are similar to traditional capitation payments except that (1) the payment amounts may be higher for individual patients who have more chronic conditions, and (2) the average payment amounts may be adjusted up or down based on quality scores.
Although a monthly payment for each patient gives a primary care practice greater flexibility to deliver different services and a more predictable revenue stream than paying fees for each individual service delivered, this approach fails to solve all of the problems with current payment systems, and it also creates new problems that do not exist under fee-for-service:
- Payments may or may not be sufficient to cover the cost of high-quality care for practices with higher-need patients. Most proposals for capitation and population-based payments set the payment amounts at levels designed to generate the same amount of revenue the practice has been receiving from fee-for-service payments, and in some cases less. This means that if the fee-for-service revenue was inadequate to cover the cost of high-quality care, it is likely that the capitation payments will also be inadequate. In addition, the payments are not adjusted for changes in patients’ acute needs, for the severity of chronic conditions, or for non-medical barriers to care, so a practice may receive even less revenue under population-based payments than it would have under fee-for-service. This could force primary care practices to avoid caring for high-need patients.
- Payments are higher than necessary for patients who need only a small number of primary care services. Even if the monthly payments are adequate on average to cover a practice’s costs, the payment over the course of year for a patient who is healthy will be much higher than what the patient or their insurance plan would have paid under fee-for-service (even if fees had been increased to better cover the costs of delivering high-quality care). That can discourage patients or their employers from participating.
- There is even less assurance that patients will receive high-quality care. As with other pay-for-performance systems, adjusting capitation payments based on average quality performance does not assure that each individual patient receives high-quality care. Moreover, in contrast to fee-for-service, under population-based payment there is no financial penalty to a primary care practice if it delivers fewer services to a patient, and there is no higher payment if the practice’s costs increase, so patients may have greater difficulty receiving services they need.
A Patient-Centered Payment System for Primary Care
Essential Characteristics of a Patient-Centered Payment System
Clearly, a different approach is needed that will actually solve the problems of the current fee-for-service payment system for both primary care practices and patients without causing new problems for either. This section describes the details of a Patient-Centered Primary Care Payment system that has four essential characteristics:
The Payment for Each Patient is Based on the Services That Patient Needs and Wants to Receive. Not every patient will need or want the same services from a primary care practice or to have them delivered in the same way:
- Some healthy patients may want the primary care practice to help them manage their preventive care needs, while others may choose to do that themselves and only use the primary care practice when acute problems arise.
- Some patients with a chronic condition may want the primary care practice to help them manage that condition; others may need or want a specialist to do so.
- Some patients may prefer to receive some services through telehealth methods while others may not want to or be able to do so.
- Some patients may have multiple injuries or acute problems during the year that need diagnosis and treatment, while others may have none.
In Patient-Centered Primary Care Payment, patients (and those paying for their healthcare services) are not expected to pay for services they do not receive; primary care practices are not prevented from delivering sufficient, appropriate services because there is no payment for them; and primary care practices are not expected to provide more or different services to higher-need patients without adequate compensation for doing so.
The Payment for Each Patient Ensures That Each Patient Receives High-Quality Care in the Most Efficient Way. An individual will be far more willing to utilize primary care to maintain their health and address their chronic and acute healthcare problems if they know they will receive the care that is most appropriate for their specific needs. This requires that a primary care practice deliver care to each patient that meets quality standards appropriate for that individual patient. It is also important to deliver high-quality care efficiently, including avoiding the use of unnecessary services and unnecessarily expensive services, and minimizing the amount of time the patient has to spend away from work, school, or other activities.
The Payment Amounts Are Adequate to Cover the Cost of Delivering Services to Each Patient in a High-Quality Way. No business can deliver a high-quality product unless it is paid enough to cover the costs of producing that product; similarly, a primary care practice cannot be expected to deliver the kinds of services each patient needs in a high-quality way unless the payments it receives for its services are sufficient to cover the costs of doing so. The only way to know if payments are adequate is to determine what it costs to deliver high-quality care.
The Payments Are Affordable for Patients With and Without Insurance. Patients can only benefit from high-quality primary care if they use it, and they will only use it if they can afford to do so. A Patient-Centered Primary Care Payment system should make primary care services as affordable as possible for all patients who can benefit from them.
Method of Payment
Different Types of Payments for Different Types of Services
Although every primary care practice delivers preventive care, acute care, and chronic disease care, each of its patients will need a different combination of those services, and different practices will have patients with different sets of needs. Moreover, not every patient will want to receive all of these services from the primary care practice.
Consequently, the most patient-centered way to pay for primary care is to have separate payments for each category of services. Moreover, because the services in each category should be delivered in different ways, different methods of payment will be needed in each category.
Monthly Payments for Wellness Care Management
Maintaining and improving one’s health is a continuous process that occurs throughout the course of each year. Patients who need multiple preventive care services or who have failed to keep up with preventive care will need to take more actions than others during the course of the year, but it will generally be necessary and/or desirable for this to be spread out over a period of time rather than occurring all at once. Consequently, a primary care practice that is assisting individuals with wellness and preventive care will need to be able to provide support to each patient throughout the course of the year.
The nature of the support will differ for different patients. For example, some patients will need or want education and assistance to be delivered in person while others will prefer virtual assistance, and some patients will need more support than others in order to successfully follow a wellness and prevention plan. A key component, however, is proactive outreach to each patient to ensure they understand and are able to obtain the appropriate preventive care and screening services in a way that is feasible for them. In addition, patients who need preventive care services from other providers will generally benefit from having the primary care practice oversee and coordinate those services to avoid duplication and resolve conflicting recommendations.
It is impossible for a primary care practice to deliver this kind of ongoing, customized, proactive wellness support if it is only paid fees for narrowly-defined episodic services such as office visits with physicians. Although some aspects of wellness care must be provided by a physician, many aspects can be delivered effectively by other types of staff in the primary care practice. Consequently, payments for wellness care must provide the flexibility to deliver services in the most effective and efficient way possible.
Since the “service” of wellness care should be continuous and flexible, primary care practices should receive a monthly Wellness Care Payment for each patient. The monthly payment would only be for wellness care management, not for any specific procedures, tests, or treatments the patient needs as part of their wellness plan, such as immunizations, mammograms, colonoscopies, etc. Payment for these other services should be made using separate service-specific fees, as discussed further below.
A patient who does not want wellness care support from the primary care practice should not have to pay for it. For example, some patients may prefer to only receive acute care from the primary care practice, and to obtain all or most of their wellness care from other sources (e.g., from a gynecology practice). Consequently, the primary care practice should only receive a Monthly Wellness Care Payment for a patient who explicitly enrolls with the primary care practice to receive wellness support.
There is at least one group of patients for whom the monthly payment for wellness care will need to be higher because the time involved in helping them will be significantly larger. Patients who have experienced a serious illness or injury and require an extended period of time to regain their health can benefit from assistance from their primary care practice during the recovery process. This is particularly true if there are multiple specialists or other providers involved in the recovery process, since the primary care practice can play an important coordination role. This “transitional care management” is more similar to wellness care management than to either acute care or chronic condition management, but because it is much more intensive, the primary care practice should receive a higher Wellness Care Payment for a patient during a month when they are recovering from a serious illness, injury, or medical procedure. In general, the higher payment would only last for a month, unless the recovery period continues for a longer period of time.
Monthly Payments for Chronic Condition Management
A patient who has been diagnosed with one or more chronic diseases such as asthma, diabetes, or hypertension will need to have a treatment plan involving a combination of medications and lifestyle changes that are designed to reduce the severity of symptoms caused by the chronic condition, to prevent exacerbations of the condition and associated complications, and ideally to slow the progression of the disease. Most patients will need education and assistance from the primary care practice in order to design a successful treatment plan and successfully adhere to it, and the practice will need to adjust the plan from time to time as the patient’s needs change and as new evidence about the effectiveness of alternative treatments becomes available. In addition, even with the most effective treatment plan, some patients will experience exacerbations of their condition during the course of the year, and it will be important for the primary care practice to identify those exacerbations as quickly as possible and take appropriate action in order to avoid more serious problems from occurring.
This process of treatment planning, education, assistance, monitoring, and response to problems must be continuous and proactive. Although patients who experience exacerbations will need additional time and assistance from the practice, it is problematic to pay the practice more when exacerbations occur (as is the case in the current fee-for-service system), because the practice is then penalized financially when it is able to prevent exacerbations from occurring. In addition, although development and adjustments to a treatment plan for a chronic condition must generally be done by a physician or other clinician, services such as education, assistance, and monitoring can often be performed effectively by nurses or other types of staff in the primary care practice.
Consequently, payments for chronic condition management need to support continuous care throughout the year, to provide flexibility for services to be delivered in the most effective and efficient way possible, and to encourage prevention of exacerbations. The primary care practice should receive a Monthly Chronic Condition Management Payment for each patient with a chronic condition.
- The patient with one or more chronic conditions will still need basic wellness and preventive care in addition to assistance in managing their chronic conditions, so the monthly payment for chronic condition management would be in addition to the monthly payment for wellness care.
- The monthly payment would only be for chronic care management, not for any specific procedures, tests, or treatments the patient needs as part of their treatment plan; these other services would be paid for through service-specific fees.
Not every patient with a chronic condition will want the primary care practice to provide assistance in managing it. Some patients may need or want to receive that support from another practice that specializes in the patient’s condition(s), particularly patients with severe conditions and patients for whom standard treatments are not effective or have problematic side effects. Consequently, the primary care practice should only receive a monthly Chronic Condition Management Payment for a patient who explicitly enrolls with the primary care practice to receive chronic care management. A patient receiving chronic care management from a specialty practice may still want to receive their general wellness care and acute care from the primary practice (and the specialty practice may be unable or unwilling to provide those other services), so having a monthly payment that is specifically tied to chronic condition management allows the primary care practice to be paid only for preventive care and/or acute care if those are the only services the patient is receiving, while being paid adequately if the patient is receiving all three types of services.
In addition, some patients with a chronic condition may need to temporarily receive proactive management services for that condition from a specialty practice rather than the primary care practice, such as when the patient experiences an acute condition that complicates management of the chronic condition (e.g., the patient becomes pregnant and the medications she had been taking for the chronic condition are problematic during pregnancy). In these cases, the patient can temporarily stop receiving chronic condition management services from the primary care practice and then begin receiving them again when the specialty care is no longer needed. Since the payments are monthly, the primary care practice can receive the monthly payments only during the months when the practice is actually providing the services.
Patients Eligible for Chronic Condition Management Payments
A patient with any chronic disease or long-term condition that requires a significant amount of proactive care should be eligible for this payment. This would include diseases that are commonly the focus of primary care initiatives, such as asthma, COPD, depression, diabetes, and hypertension, as well as chronic conditions that often do not receive appropriate attention, such as chronic migraines, and osteoarthritis. In addition, conditions such as obesity, smoking, and substance abuse should be included since they will require proactive management over an extended period of time.
Trying to precisely define which conditions qualify for the payment will only add administrative burden for the practice and the payer, and will be unlikely to lead to better quality care. It would be better to be inclusive initially, and then later exclude specific types of conditions if they are being used as the basis for billing for chronic care management when it is unlikely that any significant regular or proactive services are needed. If there is evidence that a primary care practice is abusing this flexibility, that practice could be excluded from the Patient-Centered Primary Care Payment system rather than complicating the system for all primary care practices.
Higher Payments for Specific Subgroups of Patients
There are two types of patients for whom the monthly payments will need to be higher because the time involved in chronic condition management will be significantly larger:
Higher Payments for Patients With a Newly Diagnosed or Treated Chronic Condition. A primary care practice will need to spend a significant amount of time with a patient who has been newly diagnosed with a chronic condition in order to develop the most effective treatment plan for the patient and to provide education and assistance to the patient in implementing that plan. A large amount of time will also be needed if a new patient comes to the practice who has been previously diagnosed with the chronic condition by another practice or hospital, but the patient has not been receiving treatment for the condition or the previous treatment has not been effective; in these cases, the primary care practice will need to spend time to ensure the condition has been diagnosed correctly and to design a new treatment plan that will be effective. A higher monthly payment will be needed during at least the initial month following diagnosis or enrollment in order to support this additional time.
Higher Payments for Patients With a Complex Condition. Some patients have a combination of chronic conditions or other characteristics (often referred to as “social determinants of health”) that (1) make it more difficult to develop an appropriate and feasible treatment plan in the first place, and/or (2) make the patient more susceptible to serious exacerbations or complications. For these patients, significantly different or more intensive approaches are needed for preventing exacerbations/complications and for responding when they do occur. Higher payments will be needed to enable adequate time to be spent in providing the more intensive level of care management and assistance these patients require.
Patients should not be considered to have a complex condition simply because they have multiple chronic diseases; many comorbidities occur commonly and primary care practices routinely manage the care of those comorbidities in a coordinated way. For example, a high percentage of patients with diabetes also have hypertension and/or hyperlipidemia, and the appropriate treatment for patients with diabetes includes management of hypertension and hyperlipidemia, so a patient who has two or more of these conditions should not be classified as having a complex condition solely on that basis. On the other hand, a patient who has no chronic diseases other than diabetes, but who has other characteristics that make standard approaches to treatment and management of diabetes very difficult or impossible (e.g., blindness, deafness, paralysis, homelessness, illiteracy, etc.), will require significantly more time and assistance, so such a patient would generally be appropriate for this “complex condition” category. A patient who has two chronic diseases that co-occur less frequently and where the standard approaches to treating each disease can be in conflict would also be appropriate for this category.4
Because of the diversity of factors that can make delivery of care more difficult, no fixed set of eligibility rules should be established for this category; instead the primary care physician should be able to make the determination as to whether an individual patient is appropriate for this category and document the basis for that determination. (Patients with an advanced illness can also be included in this category, but ideally, they should receive comprehensive, multi-disciplinary palliative care services, either from the primary care practice or a palliative care provider, that are supported by payments specifically designed for palliative care.)
Fees for Non-Emergency Acute Events
Patients who are receiving good preventive care and chronic disease management will still have accidental injuries and acute illnesses such as colds or urinary tract infections during the course of the year that are not emergencies and can be effectively treated by a primary care practice. In addition, many patients will experience symptoms such as pain, dizziness, or fever that could be caused by either a minor or major health problem, and a primary care practice can and should promptly diagnose the cause of such problems and determine what, if any, treatment is needed. In general, these acute events will require some type of “visit” with the primary care physician, either in person or through a video or audio connection, in order to determine an accurate diagnosis and prescribe appropriate treatment.
Since acute events will occur unpredictably during the course of the year, the primary care practice needs to be staffed and organized in a way that enables it to provide these visits quickly when a patient does experience such an event. This means that the practice will have to incur a minimum level of cost every week to maintain that readiness even if relatively few of its patients actually experience an acute event during the course of the week. From the primary care practice’s perspective, it might seem that a monthly payment for each patient would be preferable to visit-based payments because it would provide a more predictable revenue stream that would better match the costs for staff and facilities that it would incur on a regular basis. However, the practice may also need to incur extra costs (such as additional hours for part-time staff or overtime for salaried staff) if a relatively large number of patients need care during the week, and a monthly payment would provide no additional revenue to cover these extra costs.
From the patient’s (and payer’s) perspective, a monthly payment would mean that patients who experience many acute events would be paying less than the cost of the services they received, and patients who experience few or no acute events would effectively be paying for services they did not need or receive and subsidizing the care of those who did have many acute events. Moreover, if patients pay nothing extra for a visit, some of them will likely request visits more often than necessary, and if the practice’s revenue did not depend on how many visits it scheduled, it would have a much weaker incentive to see patients quickly. As a result, monthly payments are not a patient-centered approach to payment for acute care.
In contrast to preventive care and chronic care, acute care is fundamentally reactive, episodic, and short-term in nature, so the primary care practice should receive an Acute Care Visit Fee when it provides diagnosis and treatment for a new acute event affecting a patient.
Although diagnosing and treating a new acute event requires some kind of “visit” with the patient, this is different than what has traditionally been described as a “visit-based payment” in fee-for-service systems:
- Patients who are receiving preventive care and/or chronic condition management services from the practice will likely also have visits with practice staff related to those services, but the cost of those visits will be supported by the monthly Wellness Care and Chronic Condition Management Payments. In contrast, if a patient with a chronic condition has an acute event such as an injury or a new symptom that they have not experienced before, the practice should be paid an additional amount for the visit needed to diagnose and treat that acute problem.
- Conversely, the fact that an additional fee is paid specifically for a visit to diagnose and treat an acute problem does not mean that the visit to the practice has to be limited to the acute problem. It may well be convenient for the primary care practice to address some of the patient’s wellness care or chronic condition management needs on the same day that an acute problem is being addressed, and it may be necessary or appropriate to do so if changes in wellness care or chronic condition management are needed because of the acute event. This will require the practice to spend more time with the patient than what would have been necessary solely to address the acute issue, but if the patient has enrolled with the practice for wellness care or chronic condition management, that extra time would be supported through the monthly Wellness Care and Chronic Condition Management Payments, not through the Acute Care Visit fee.
The Acute Care Visit Fee should be designed to allow sufficient time for the physician to examine the patient, correctly diagnose the condition, and develop an appropriate treatment plan through a shared decision-making process with the patient. This can generally be done in 30 minutes for most types of acute problems that typically arise in primary care. If the physician needs to spend significantly more time than this because of the complexity of the specific acute issue that is being addressed, then the physician would be paid two Acute Care Visit Fees. If it was appropriate for the patient to return for a second visit for the same acute problem (e.g., to verify that a prescribed medication had fully addressed the problem), then there would be a second Acute Care Visit Fee for that second visit. This would be a simpler, more straightforward process than trying to define different payment amounts for different amounts of time, and it would avoid creating a financial penalty for a physician who spends adequate time to address the patient’s needs during a single visit rather than asking the patient to come back for second visit on another day.
Acute Care Visit Fees for Patients Receiving Chronic Condition Management Services
The Acute Care Visit Fee should not be paid if the patient’s problem is clearly an exacerbation of a chronic disease and if the practice is receiving a monthly Chronic Care Management Payment for the patient, since the monthly payment is intended to cover the costs of both preventing exacerbations of the chronic disease and addressing exacerbations when they occur. For example, if the patient has asthma, and the practice is receiving a monthly Chronic Condition Management Payment specifically for asthma, then if the patient experiences an asthma attack and needs assistance or treatment from the primary care practice, the primary practice would not receive an Acute Care Visit Fee for providing that assistance/treatment. In fact, high-quality care for asthma includes development by the practice and patient of an “asthma action plan” defining what the patient and practice will do to prevent and treat asthma attacks, and one of the elements of the plan will likely be to specifically encourage the patient to contact the practice as soon as possible when an asthma attack appears to be occurring, rather than waiting until it becomes severe.
There will be many cases in which it will be uncertain whether a particular acute problem was caused by a patient’s chronic disease, and there will also be cases in which the acute problem triggers an exacerbation of the chronic disease. In these cases, the primary care practice should have the discretion to bill for an Acute Care Visit Fee depending on what they believe is most appropriate in the circumstances. Trying to precisely define which situations qualify as acute events and which do not will only add administrative burden for the practice and the payer, and will be unlikely to lead to better quality care. If there is evidence that a primary care practice is abusing this flexibility, that practice could be excluded from the Patient-Centered Primary Care Payment system rather than complicating the system for all primary care practices.
Need for Further Risk Adjustment
As shown in Figure 1, the additional monthly payments for patients with chronic conditions, the higher monthly payments for patients with complex conditions, and the additional fees for patients with new acute problems result in the practice receiving a higher total payment during the month for a patient who has greater needs. This is analogous to what is accomplished in population-based payment systems where a single monthly payment for the patient is “risk adjusted” based on characteristics of the patient.
FIGURE 1
Differences in Monthly Primary Care Practice Revenues
for Different Types of Patients
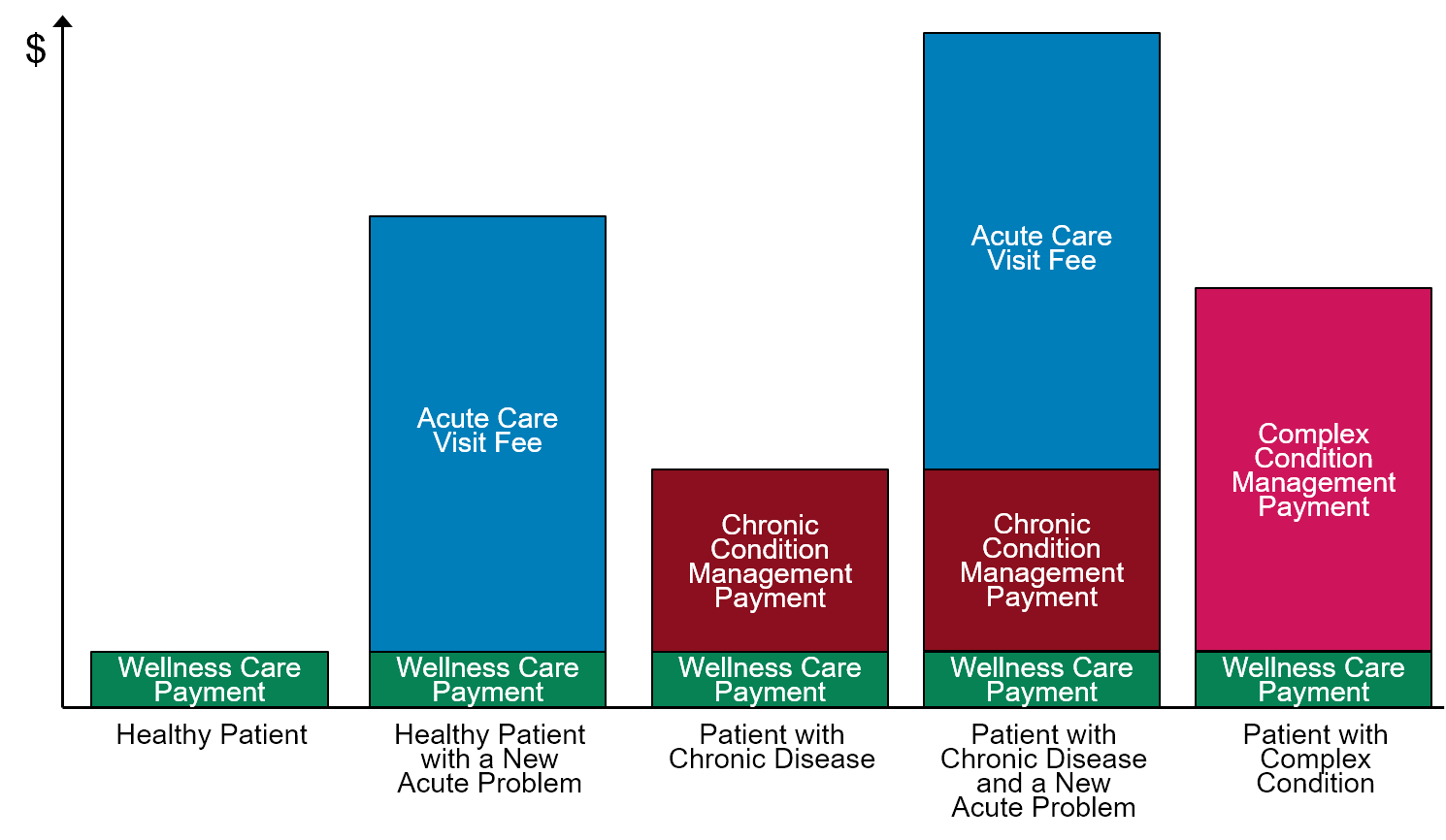
However, in most risk adjustment systems, there is no change in the payment amount for a patient who has an acute problem, for a patient with a newly diagnosed chronic disease, or for a patient who has non-medical characteristics that make their care more complex. As a result, the payments to the primary care practice under Patient-Centered Primary Care Payment would better match the actual differences in the time that a primary care practice would spend with different patients.
Fees for Individual Procedures and Tests
The payments described above are designed to pay for three specific types of services – wellness care, management of chronic conditions, and visits to diagnose and prescribe treatment for new acute care issues. As part of the treatment or management plans developed in any of these areas, the primary care practice may perform a procedure such as an immunization or injection, a suture or excision, or therapy for a chronic condition. It is beneficial for a patient to be able to receive these procedures from the primary care practice when feasible and appropriate, since it avoids the need to make a separate trip to another physician or facility and helps ensure that the patient receives the appropriate procedure in a timely way.
At a minimum, performing one of these procedures will require additional time from the primary care physician or other practice staff beyond what they would otherwise need to spend with that patient, and in most cases, the practice will need to incur out-of-pocket costs for medications, supplies, or equipment in order to perform the procedure. If the primary care practice does not receive sufficient revenue to cover the additional time and cost associated with performing these procedures, it will be unable or unwilling to deliver them.
In addition, it is helpful if the patient can receive basic laboratory tests at the practice, such as measurements of the patient’s cholesterol or blood sugar levels, rather than having to make a separate trip to a laboratory and then potentially having to make a separate visit or contact with the primary care practice in order to receive the appropriate treatment based on the result of the test. Most of the common tests ordered by primary care practices can be performed at the primary care practice using equipment and chemicals designed for that purpose without any special licensing. However, there is a fixed cost for acquiring the testing equipment, there is a cost for the chemicals needed for each test, and time is needed to have the test performed by a trained staff member. If the primary care practice does not receive sufficient revenue to cover these costs, it will be unable or unwilling to perform them.
Since only a subset of patients will need these procedures and tests and since the cost of performing each procedure and test will differ, the primary care practice should receive an additional fee when an individual patient receives a procedure or test. The amount of the fee should be adequate to cover the costs of delivering that type of procedure or test.
Payments for Integrated Behavioral Health Services
There is growing recognition that primary care practices need the ability to deliver some types of behavioral health services so that patients who have both behavioral health needs and physical health needs can have them treated and managed in a coordinated way. Although primary care physicians can and do provide a basic level of behavioral health counseling to patients as part of office visits for other medical issues when needed, many primary care practices have not had appropriate staff to provide additional or more intensive behavioral health services to patients because of barriers in the current payment system – either there is no payment at all for such services, or the payments that do exist are too small and/or too narrowly defined to support the kinds of services the primary care practice would be able to deliver.5
There are two basic approaches for delivering behavioral health services in primary care practices – the Collaborative Care (IMPACT) Model6 and the Primary Care Behaviorist Model.7 Both of these models are based on having one or more individuals with behavioral health expertise working for the practice who can provide in-person and/or virtual counseling and care management to patients with a suspected or diagnosed behavioral health problem such as depression, anxiety, or substance use disorder. Patients with severe conditions would need to be referred to a specialized behavioral health care provider rather than receiving treatment from the primary care practice, but the primary care practice’s behavioral health staff could help ensure that the care the practice is providing for these patients’ physical health problems is coordinated with the behavioral health treatment they receive from the other provider(s).
It is problematic to pay for these integrated behavioral health approaches using fees for counseling sessions. There is typically a high no-show rate for such sessions that can cause fee-based revenues to fall below the cost of employing the counseling staff, and paying fees for individual sessions can encourage scheduling more sessions than necessary. In addition, it is important to enable primary care physicians to make a “warm handoff” to the behavioral health staff when a patient visits the practice for medical reasons and the physician identifies the need for behavioral health care. This can only occur if the behavioral health staff’s schedule is not completely filled each day, and under a fee-based system, open time on the schedule means a loss of revenue.
Monthly payments would provide the practice with predictable revenue to support integrated behavioral health services and the ability to maintain open times on the schedule. However, it would be undesirable if monthly payments were limited to patients who have been formally diagnosed with a behavioral health condition; the physician should not be forced to assign a formal “mental health” diagnosis to a patient if they believe that would be problematic for the patient or if the physician is not sure what diagnosis to assign.
The most appropriate approach would be to treat basic behavioral healthcare services as an additional component of the primary care practice’s wellness care services, since many patients will need some level of behavioral health support at some point in time. A primary care practice that delivers integrated behavioral health services should receive a monthly Integrated Behavioral Healthcare Payment in addition to the monthly Wellness Care Payment for each of the patients who has enrolled for wellness care from the practice.
Payments for New Patients
The payments for wellness care and chronic condition management described above would only be for patients who explicitly enroll with the practice to receive these proactive services on an ongoing basis. A primary care practice will want to ensure that it can meet a patient’s needs before enrolling them for ongoing services, and the patient may be unwilling to enroll until they have a chance to discuss with the physician whether the practice will deliver the services the patient needs in a way that is convenient for the patient. Consequently, most new patients will need at least one initial visit with the practice before enrollment occurs.
The current fee for service system pays a higher amount for the initial visit with a new patient than for visits with established patients, and the initial visit payment is higher for new patients who have multiple, complex problems than for those who do not. There does not seem to be any compelling reason to change this approach to paying for the initial visit, since if the practice can meet the patient’s needs, it will be in both the practice’s interest and the patient’s interest for the patient to enroll with the practice and begin receiving the proactive, high-quality care that would be supported by the monthly payments for enrolled patients.
Payments for Services to Non-Enrolled Patients
Patients who are unwilling or unable to enroll with a primary care practice for ongoing wellness care or chronic condition management services may still want or need to receive occasional services for acute conditions, chronic condition exacerbations, etc. If a primary care practice provides a service to one of these patients, the practice should be paid for doing so; current fee-for-service payments can continue to be used for this purpose.
Billing and Payment for Services
The simplest and best way to operationalize the new payments for wellness care, acute care, chronic condition care, and behavioral healthcare for patients who have health insurance is to create a billing code for each of the new payments. Each of these services/payments would need to be assigned a CPT® (Current Procedural Terminology) code by the American Medical Association’s CPT Editorial Panel. Alternatively, HCPCS (Healthcare Common Procedure Coding System) Level II Codes could be created by the Centers for Medicare and Medicaid Services (CMS) HCPCS Workgroup. New CPT codes and HCPCS codes are created every year in order to allow physician practices to bill for new types of procedures and services,
Specifically:
- A new CPT code (“XX010”) would be created to represent one month of Wellness Care services for a patient who has explicitly enrolled with the practice to receive wellness and preventive care. An additional CPT code (“XX011”) would be created to allow a higher payment during the month for a patient who has been discharged from a hospital or is recovering from a serious illness.
- A new CPT code (“XX020”) would be created to represent a visit in which a patient receives diagnosis and treatment planning services for a new acute symptom or problem. (The “visit” could either be in person or through electronic means, as appropriate.)
- A new CPT code (“XX031”) would be created to represent one month of Chronic Condition Management services for a patient who has explicitly enrolled with the practice to receive these services. An additional CPT code (“XX030”) would be created to allow a higher payment during the initial month of care for a patient with a newly diagnosed/treated chronic condition, and another CPT code (“XX032”) would be created to allow higher payment on an ongoing basis for patients who have a complex condition.
- A new CPT code (“XX012”) or a code modifier (“XX010-BH”) would be created to provide an additional monthly payment for each patient who has enrolled in the primary practice for wellness care if the practice has the capacity to deliver integrated behavioral health services.
The definitions of the new CPT codes should not specify exactly what wellness or chronic condition management services the patient would have to receive during the month or what services must be provided during the acute care visit in order for the practice to be paid. In particular, the practice should have the flexibility to deliver services in person or through electronic means, to have services delivered by the physician, a nurse, or other member of the practice staff, etc. Section 4-C describes the method that would be used to ensure that appropriate care was being delivered in return for payment.
The physician would make the determination as to which specific CPT code was appropriate based on the patient’s characteristics and the type of service being delivered. For example, if the physician determined that the patient had a complex chronic condition that was eligible for the higher chronic condition management payment, the physician would bill using the appropriate code, while maintaining appropriate documentation for doing so in the patient’s clinical record.
The primary care practice would submit the appropriate CPT code to a patient’s health plan when that patient received wellness care, acute care, or chronic care management services from the practice, and the health plan would pay the practice the amount assigned to each of those codes (Section 4-D discusses how the payment amounts should be determined). For example:
- If a patient who is enrolled only for wellness care receives no other services during the month, the practice would submit a bill with the XX010 code to the patient’s health plan for the month.
- If a patient who is enrolled for wellness care also visits the practice for an acute problem, the practice would submit a bill with both the XX010 and XX020 codes. If the patient also receives a procedure to address the acute problem, the practice would include the appropriate billing code for that procedure on the claim form in addition to the other codes.
- If a patient has a chronic disease and enrolls with the practice for chronic condition management, the practice would submit a bill each month with both the XX010 and XX031 codes.
- If a patient has not enrolled with the practice for ongoing wellness care or chronic condition management services and the practice delivered a procedure or other service to the patient, then the practice would bill for that service the same way it does today using the appropriate existing billing code for the service.
Since new CPT and HCPCS codes are created every year, every physician practice’s billing system has the capability to use new codes, and every health insurance company’s claims payment system has the capability of processing claims with new codes, so this approach would involve minimal administrative costs for the primary care practice and the health insurance company.
If a primary care practice submits the monthly billing code for either Wellness Care or Chronic Condition Management, it would not bill for any of the current CPT codes for Evaluation and Management (E/M) services to established patients (i.e., 99211-99215) during that month. If the health insurance plan received a claim with one of these codes and also a claim with an XX01x, XX02x, or XX03x code for the same patient during the month, it would only pay for the latter codes.
Enrollment of Patients
The primary care practice would only be eligible to receive the new payments for patients who had enrolled with the practice to receive ongoing services, so the practice would only submit a claim form with one of the new billing codes for a patient if that patient had, in fact, enrolled with the practice for ongoing care. The practice would only be eligible to receive chronic condition management payments for a patient if they had an eligible chronic condition, so the practice would only submit billing codes for chronic condition management if the practice had diagnosed the patient with a chronic condition and the patient had agreed to receive regular, proactive care management for that condition from the practice.
The enrollment process should be carried out by the primary care practice, not by the patient’s health insurance company. No patient should be “attributed” to the practice by a health insurance company without the knowledge and consent of the patient and the primary care practice. A patient would have to explicitly tell the primary care practice that it wanted to enroll to receive proactive care from that practice, and the practice would need to ensure that it had the capacity to provide the appropriate services to address the patient’s needs before agreeing to enroll that patient.
It will be important for patients to understand that enrolling with the primary care practice to receive proactive wellness care or chronic care management services from the practice does not mean that the primary care physician will be serving as a “gatekeeper” who will determine whether the patient can receive any other kind of services, unless the patient has enrolled in an HMO-type insurance plan and the primary care practice has agreed to play the gatekeeper role for patients in that insurance plan.
The practice would inform the patient’s health insurance company that the patient had enrolled by submitting claims for the monthly wellness care and/or chronic condition management payments.8 This process is far less burdensome for both the primary care practice and the health plan than the complex and problematic attribution systems that have been used by Medicare and other payers to make monthly “population-based payments” to primary care practices.
A patient should also be able to disenroll from receiving proactive care from the practice if they are no longer able or willing to receive it. Since the wellness care and chronic condition management payments would be billed for and paid monthly, a patient could disenroll at the end of any month if they wished to, and the primary care practice would then stop submitting bills for the monthly payments for that patient. As discussed earlier, it may be appropriate for some patients to stop receiving chronic condition management services from the practice temporarily while they are receiving services for that condition from a specialty practice (e.g., during pregnancy), and the monthly payment structure easily allows that to occur.
Accountability for Quality and Utilization
The second key characteristic of a Patient-Centered Primary Care Payment system is ensuring that each patient receives high-quality care in the most efficient way. This can only be done if there is a clear definition of what “quality care” from a primary care practice means for each individual patient and if there is a mechanism for assuring that quality care is being provided without the use of unnecessary and unnecessarily-expensive services.
The Problems With “Outcome-Based Payment”
Although it would seem ideal to evaluate the quality of a patient’s primary care services based on whether the services produced a good outcome for the patient, this is impractical to do for several reasons:
- Primary care practices provide care to patients with a large number of health problems and a diversity of needs and preferences. There is no single “outcome” that would be appropriate for all patients.9
- There are no outcome measures at all for many conditions commonly managed by primary care practices, and where there are, it is generally agreed that outcomes must be assessed through multiple measures rather than one single outcome measure. For example, an international effort to define outcomes for diabetes resulted in a list of 27 separate outcome measures, ranging from glycemic control to psychological well-being.10
- In general, even when an outcome measure has been developed, there is no standard defining the minimum outcome that a primary care practice could be expected to achieve or the timeframe in which an outcome should be expected to occur. For example, in the consensus document on diabetes outcome measures, no target values were defined even for things that are routinely measured, such as blood pressure, body-mass index, and glycated hemoglobin (HbA1c). In general, it is impossible or inappropriate to expect the same outcomes for every patient because of the many differences in characteristics of patients that can affect treatment outcomes. The consensus document on diabetes outcomes defines 16 different variables needed to adjust the outcome measures in order to compare outcomes for different groups of patients.11
- When attempts are made to define target values for an individual outcome measure, they can result in worse overall outcomes for some patients. For example, diabetes quality measures have typically defined a single HbA1c target level for most or all diabetic patients, even though there is clear evidence that it is neither feasible nor desirable for every patient to achieve the same HbA1c level, and overly-aggressive efforts to reduce patients’ HbA1c levels to achieve these targets have caused serious problems for some patients.12
- Performance on most outcome measures is affected not just by the services delivered by the primary care practice, but by the willingness and ability of a patient to do what is necessary to achieve the outcome. For example, a primary care practice can prescribe appropriate medications for diabetes and encourage patients to take them, but the practice cannot force patients to do so, and a large percentage of patients do not take the medications needed to control their disease.13 Consequently, even if a desirable, patient-appropriate outcome target could be defined for an individual patient, it would be inappropriate to hold the primary care practice responsible for failure to achieve that target without controlling for the patient’s own contributions.
A Bad Alternative: Quality Measures
Even though a primary care practice cannot be held directly accountable for whether good outcomes are achieved, one would still want the practice to plan and deliver the services to each patient that are most likely to result in a good outcome for that patient.
If there is strong clinical evidence that a particular set of services will result in the best outcome for a particular patient, then it is reasonable to expect the practice to deliver those evidence-based services to the patient, or at least attempt to do so. Similarly, where there is evidence that a particular set of services is ineffective or harmful, it is reasonable to expect that a practice will avoid delivering or ordering those services, even if the patient might want to receive them.
This has led to a proliferation of quality measures, each intended to measure whether a specific aspect of a primary care practice’s services is consistent with one or more pieces of evidence regarding the right way to diagnose or treat a specific health problem. However, this approach has been ineffective in improving quality14, burdensome for primary care practices15, and potentially harmful to patients.16 Some of the reasons for this include:
- Most quality measures are based on whether a specific approach to services has been used or a specific standard of quality has been met for all patients who have a particular disease or are in a specific demographic group, even when evidence clearly indicates that different services or standards are appropriate or necessary for a significant subset of those patients.17 As a result, one cannot expect any primary care practice to meet these quality measures 100% of the time, and there is no way to determine whether a difference in performance between practices is due to differences in the characteristics of the patients they treat or differences in the actual quality of care they deliver.
- The quality measures typically define a specific threshold to distinguish “good quality” care from “poor quality care.” The only thing that affects the measure is the number of patients on either side of that threshold, so care can get worse for the patients who are receiving “good” care and care can get better for patients who were receiving “poor” care without causing any change at all in the quality measure.
- If the patient is unwilling to accept the services required to meet the quality measure, or if there are barriers that prevent the patient from obtaining those services (e.g., an allergy to a medication or inability to afford the medication), then the primary care practice will need to deliver or order alternative services. Most quality measures provide no mechanism for excluding these patients from the measure, so care that is more consistent with patient preferences and needs can appear to be worse on the quality measures.
Because primary care practices deliver care for a wide range of different health problems and a wide variety of patients, measuring quality in this way for every problem and every type of patient would require hundreds of different measures. The burden that using a large number of measures causes for primary care practices has led to efforts to reduce the number of measures used, but this does not resolve the problems with the individual measures nor does it provide any way to assure quality for the many patients whose care is not measured at all.
Another Bad Alternative: Prior Authorization
For many types of health problems and patients, there is no clear evidence as to what services are effective and which will result in the best outcome for particular types of patients. As a result, some physicians use far more services, or far more expensive services, than others. There may be no evidence to support this, but there may also be no evidence showing that it is harmful.
In an effort to prevent primary care practices from ordering or delivering unnecessary and unnecessarily-expensive services, many health insurance companies require a primary care physician to obtain “prior authorization” from the insurance company before the company will pay for certain kinds of medications, tests, or procedures ordered or delivered by the physician. These prior authorization processes are extremely problematic18 for several reasons:
- If there is no clear evidence to guide the physician’s decision about which services to use, there is also no clear evidence to guide the health insurance company’s decision, and the insurance company has far less information about the patient’s symptoms, history, and characteristics to inform its decision than the physician does.
- As a result, there will still be variation in what services are delivered, but the variation will be driven by differences in the prior authorization rules and decisions made by different health plans, rather than differences in patient needs.
- Seeking prior authorizations from health plans and challenging inappropriate denials by the health plans requires the primary care practice to spend a large amount of time and money19 that does nothing to improve patient care. It also requires the health plan to spend money on staff to review and decide on prior authorization requests. There is no evidence that the savings, if any, from reductions in unnecessary services justifies the costs incurred by both payers and primary care practices.
- Most prior authorization requests are ultimately approved, so the process merely delays the delivery of care the patients would have received anyway. In some cases, these delays can lead to bad outcomes for patients.
A Better Way: Using CPGs/SCAMPs and SAINTs
Guidelines, Pathways, and SCAMPs
Clinical Practice Guidelines (CPGs) represent a more comprehensive, efficient, and patient-centered mechanism for achieving good patient outcomes than a list of quality measures. A clinical practice guideline assembles all of the available evidence regarding how to diagnose a symptom or treat a condition in a way that is likely to achieve the best outcome for each patient.20 Moreover, in contrast to the one-size-fits-all nature of quality measures, a CPG encourages and guides appropriate customization of services to patients with different characteristics based on available evidence.
Since clinical practice guidelines define which services are inappropriate as well as which services are appropriate, they can reduce use of unnecessary services in a more patient-centered way than burdensome and problematic prior authorization processes. In order to reduce variation, the guidelines can include a recommended option when there are multiple diagnostic or treatment choices and the available evidence does not indicate which option is better. The term “Clinical Pathway” is often used to describe a set of guidelines that recommend the use of a specific approach when the evidence is unclear or where multiple options have equivalent benefit.21
Clinical practice guidelines and pathways have been successfully used to improve quality and reduce variation in a variety of settings22, and studies have found that primary care physicians would be willing to use guidelines if they are designed and implemented appropriately.23 In order to avoid re-creating the problems of quality measures and prior authorization, effective clinical guidelines/pathways for primary care need to meet four criteria:
- Ease of Use. The guidelines must be structured so they are easy for primary care physicians to use. The most useful versions of guidelines/pathways are integrated directly into the physician’s EHR (so they do not require re-entering data about the patient), they address all of the inter-related decisions the physician will be making (e.g., about both diagnosis and treatment) rather than forcing the physician to consult multiple separate guidelines, and they are structured as flowcharts or decision trees so the physician can quickly determine which specific recommendations are most applicable for the specific patient the physician is treating.
- Ability to Deviate. Physicians must have the ability to depart from the guidelines/pathway when there are good reasons to do so.24 For many types of patients, there is not strong evidence as to what approach to diagnosis or treatment would achieve the best result, so no guideline can dictate what should be done for every patient.25 In particular, when patients have multiple chronic conditions, guidelines designed for care of individual diseases may not be appropriate.26 In addition, the patient may be unwilling or unable to accept the services recommended by evidence, in which case a different set of services will be needed.
- Documentation for Deviations from Guidelines. In order to use evidence where it is applicable and to reduce unnecessary variation, deviations from the guidelines/pathways should only occur for good reasons. Consequently, there must be a mechanism for physicians to document the reasons for deviation if the guideline is not followed for a specific patient.
- Modification and Expansion of Guidelines. There should also be a process for modifying or expanding guidelines to address the situations where physicians feel the guidelines do not apply or would be problematic for particular types of patients. Clinical data from electronic health records can be collected and analyzed to determine whether the care that was delivered outside the guidelines resulted in good outcomes for the patients, and if so, the guidelines and recommendations can be revised accordingly. This process can generate new evidence more quickly and cost-effectively than randomized control trials, and it may be the only feasible way to generate evidence about how to treat health problems that occur infrequently and patients with special characteristics.
A Standardized Clinical Assessment and Management Plan (SCAMP) is a form of clinical practice guideline/pathway that achieves these goals. It is explicitly designed to allow deviations in appropriate situations. In addition, there is an explicit process for using information about the circumstances and reasons for deviations and the outcomes of those choices in order to improve the guidelines.27 SCAMPs have been successfully used to improve guidelines and outcomes for patients in a number of areas such as evaluating chest pain, diagnosing food allergies, etc.28
To be successful in supporting patient-centered care, CPGs and SCAMPs must be developed and refined by clinicians, not by health plans. Clinicians will be more likely to utilize and adhere to clinician-developed CPGs/SCAMPs than rules or pathways developed by payers or other entities where cost considerations may have taken precedence over patient outcomes in defining recommendations.29 In addition, a CPG/SCAMP developed by clinicians can be used for all patients, regardless of payer.
A SAINT
Although greater use of CPGs/SCAMPs in primary care would likely result in greater use of evidence-based services and reduce the use of unnecessary services, this would not be sufficient for achieving the best outcomes for patients, because the CPGs/SCAMPs do not directly ensure that an individual patient’s most important needs are being adequately addressed:
- Although the guidelines can help ensure the right services are being used to diagnose and treat a specific patient problem, the physician has to know the problem exists in order to use the guidelines.
- In addition, the physician needs a way to know whether the patient is actually experiencing better outcomes as a result of the services that are delivered. In most cases, evidence merely indicates that the probability of achieving a good outcome is higher with one set of services than others, not that a better outcome is guaranteed. If services recommended in the guidelines fail to achieve better outcomes for a particular patient, a different approach will be needed. SCAMPs allow deviations from the guidelines in these situations, but there must also be a way to determine whether the alternative approaches resulted in good outcomes so that the guidelines can be modified appropriately.
- Most evidence-based guidelines are focused on one particular symptom or condition, and they may provide little or no guidance as to what will work best for patients who have multiple conditions. Even if each of the condition-specific approaches recommended by guidelines would be desirable, it may be impractical or impossible for a patient who has multiple conditions to take all of those actions or receive all of those services simultaneously. A method is needed for prioritizing which evidence-based actions to take and which to defer or ignore based on the goals that are most important to the patient.
Consequently, in addition to CPGs/SCAMPs, a primary care practice needs a Standardized Assessment, Information, and Networking Technology (SAINT). A SAINT provides a systematic way for a patient to provide their primary care practice with actionable information about any physical and emotional problems they are having and whether the services the practice is providing to the patient are addressing the issues that are of most concern to the patient.30
A successful SAINT will have the following characteristics:31
- Easy to Use and Affordable for the Primary Care Practice. The SAINT must allow the primary care practice to both collect and access information about patients’ needs in a way that does not require a large amount of time by the primary care physician and other practice staff and does not require a significant upfront or ongoing cost in terms of equipment and software.
- Provides Timely, Actionable Information to Guide Care. The information provided by the SAINT needs to tell the practice whether the patient has a problem now, rather than what problems may have existed in the past, and the information needs to be specific enough to allow the practice to determine what initial action to take in response.
- Enables and Encourages Patient Participation. Ideally, the primary care practice would receive information from all of the patients in the practice. However, because the information describes problems and priorities from the patients’ perspective, patients have to be both willing and able to provide the information. This not only means the SAINT has to be easy for patients to use, but patients need to feel that submitting the information will actually result in better care, and they must not be concerned that the information will be inappropriately shared or misused in any way.32
How’s Your Health is a SAINT designed specifically for primary care that meets all of these criteria:
- It operates through a web-based platform (www.HowsYourHealth.org) that is free for primary care practices and easy for patients to use.
- It generates a summary measure called the What Matters Index (WMI) that identifies which patients are experiencing problems and assesses key patient outcomes.33 The WMI has been shown to predict health care spending as well or better than other commonly-used risk stratification/prediction tools.34
- It enables patients to identify specific risk factors, concerns about their health, and problems they have had getting appropriate help so the primary care practice can better plan how to assist them.35 It can serve as the Health Risk Assessment required as part of the Medicare Annual Wellness Visit.36
- The detailed information submitted by the patient can remain confidential and the patient can decide what information to share with the primary care practice or other healthcare providers.
How’s Your Health provides information similar to other methods of surveying patient-reported outcomes, but in a more cost-effective way. It also provides more immediate information about the patient’s experience of care more cost-effectively than the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey currently used to assess patient experience37 and avoids problems associated with patient “satisfaction” ratings.38 Primary care practices can also use the system to compare their performance in achieving good outcomes for patients with the performance of other primary care practices, since the data provide a way of controlling for important differences in patient characteristics, including patient income, functional status, and other barriers to care as well as demographics and diseases.
Assuring Accountability for Quality
If (1) a patient has chosen to receive care from a primary care practice for an acute issue, or if the patient has enrolled with the practice to receive proactive wellness care or chronic condition management, and (2) the payment from the patient (or their health insurance plan) is sufficient to enable adequate time to be spent consulting clinical guidelines and monitoring patient outcomes as well as delivering services, then (3) it is reasonable for the patient (and the payer) to expect that the primary care practice will plan and deliver services in accordance with available evidence-based guidelines. If the patient is unwilling to accept those services or if there are barriers that prevent the patient from obtaining them (e.g., inability to afford a particular medication), then the practice should have the flexibility to deliver or order alternative services, but this should only occur after the patient is educated about the evidence-based services and efforts are made to overcome any barriers to using them. In addition, the practice should be expected to follow up with patients who have received evidence-based services and to monitor patients who have enrolled for proactive care to determine whether their needs are being addressed, and the practice should be able to deliver different services if the evidence-based services are not effective.
In general, if a primary care physician wants to achieve good outcomes for their patient, they will need to deliver the kinds of evidence-based services described in clinical practice guidelines, so holding the practice accountable for doing so is essentially equivalent to holding the practice accountable for outcomes. If the practice does not deliver care in a way that is consistent with the best-available medical evidence and the patient’s own needs and preferences, then the practice should not expect to be paid for that visit or service. This is the standard of quality used in every industry other than healthcare – if a business does not deliver a high-quality product or service, the business will not be paid or it will be expected to refund the customer’s money.39 It doesn’t matter how many other customers received properly-functioning products and services; if a particular customer fails to receive a high-quality product or service, that specific customer will not be expected to pay. In contrast, healthcare providers have been typically paid for the services they deliver even if one or more services failed to meet evidence-based standards of quality and necessity, or if they failed to deliver the services that were most appropriate to address the patient’s problems.
The simplest and most patient-centered method for assuring high-quality primary care services is to require that the primary care practice properly utilize appropriate CPGs/SCAMPs and a SAINT for each patient in order to bill for delivering a service to that patient. Specifically:
- Accountability for Quality in Non-Emergency Acute Care. If a patient seeks care for a new acute problem from a primary care practice, the practice would only bill for an Acute Care Visit Fee for that problem if it attests: (1) that it utilized one or more SCAMPs or CPGs appropriate for the problem, and (2) that it either (a) delivered services consistent with the guidelines or (b) documented the reasons for deviation in the clinical record (i.e., why the guidelines were inapplicable or inappropriate or that the patient had explicitly indicated that they were unwilling or unable to obtain the services consistent with the guidelines).
- Accountability for Quality in Wellness Care. If the patient has enrolled to receive wellness care from the primary care practice, the practice would only bill for a Wellness Care Payment for that patient for the current month if it attests: (1) that it was using a SAINT to identify and prioritize any problems the patient was experiencing, (2) that it had utilized one or more SCAMPs or CPGs to determine how to address any health problems and to determine what preventive care was appropriate, and (3) that the patient had either (a) received services consistent with the guidelines or (b) the reasons for deviation had been documented in the clinical record.
- Accountability for Quality in Chronic Condition Management. If the patient has enrolled to receive chronic condition management from the primary care practice, the practice would only bill for a Chronic Condition Management Payment for that patient for the current month if it attests: (1) that it was using a SAINT to identify and prioritize any problems the patient was experiencing, (2) that it had utilized a SCAMP or CPG for the chronic condition to determine what services were appropriate, and (3) that the patient had either (a) received services consistent with the guidelines or (b) the reasons for deviation had been documented in the clinical record.
- Accountability for Quality in Behavioral Healthcare: If the patient has enrolled to receive wellness care from the primary care practice, the practice would only bill for an Integrated Behavioral Healthcare Payment for that patient for the current month if it attests: (1) that it was using a SAINT to identify behavioral health problems the patient was experiencing, (2) that it had utilized one or more SCAMPs or CPGs to determine what services were appropriate, and (3) that the patient had either (a) received services consistent with the guidelines or (b) the reasons for deviation had been documented in the clinical record.
Enforcing Accountability
The primary care practice should be expected to attest that it has utilized an appropriate CPG/SCAMP and SAINT when it bills a payer or patient for a service. It should not be required to submit documentation of that to a health plan in order to receive payment. Similarly, if the practice has deviated from the guidelines, it should be expected to maintain documentation of the reasons for the deviation in the clinical record, but it should not be required to submit that documentation to a health plan.
This is the same approach that is used in current fee-for-service payment systems to assure that a physician practice has delivered the service that it is billing for. When the physician practice submits a bill for a service, it is attesting that it delivered that service to the patient; it does not have to submit any other documentation to the health plan that it did so, but it maintains documentation in the clinical record that can be used, if necessary, to show that the billing was done properly.
While it would obviously be possible for a physician to bill for a service or a month of care without actually following the recommendations of a CPG/SCAMP or without documenting the reasons for a deviation, it is similarly possible today for a practice to bill for a service without actually having delivered it. The first protection against this happening should be the patient. If patients are told that it is a good thing for primary care practices to use CPGs/SCAMPs and a SAINT, many will want to ensure their primary care physician and practice staff are doing so, and they will be less likely to continue receiving care from a practice that they feel is not using the best medical evidence to guide their care. If primary care practices provide patients with information from CPGs/SCAMPs explaining why the physician has prescribed particular treatments and the types of outcomes expected, this could encourage a higher percentage of patients to adhere to the treatment plan. Moreover, if a patient feels less compelled to look for “evidence” themselves, that could reduce the time spent by the physician and other practice staff trying to correct misinformation the patient has received from unreliable sources.
Research shows that physicians will only deviate from evidence-based guidelines in a small percentage of cases.40 Almost all deviations occur where the guidelines are inappropriate41 or where patients refuse to accept the recommended treatment.42
If a health plan has reason to be concerned that a particular primary care practice is delivering or ordering services without utilizing a CPG/SCAMP or that it is deviating from the CPG/SCAMP excessively without good reasons, it could request documentation from that practice and recoup any payments that were made inappropriately. This is the same as what is done today in fee-for-service payment systems if there is concern that a practice has been billing for a service that was not delivered.43
Adequacy of Payments
The third essential characteristic of a Patient-Centered Primary Care Payment system is that the amounts the primary care practice is paid for its services must be adequate to cover the cost of delivering appropriate services in a high-quality way. No matter what method is used to pay the practice, if the payment amounts are not sufficient to cover the cost of delivering high-quality services, the primary care practice will be forced to deliver low-quality care or go out of business altogether. Any attempt to require the delivery of high-quality care without ensuring that payments are adequate can be expected to fail.
There is very little information available on what it actually costs to deliver high-quality primary care. Information is available on how much is currently being paid for individual primary care services and how much is being spent in aggregate by Medicare and some other payers. However, information on payments and spending is not helpful, since there is widespread agreement that current payments are not adequate to cover the costs of operating primary care practices. Information on the current costs of primary care practices is not sufficient, either, since it is also generally agreed that truly high-quality primary care cannot be delivered with the levels of staffing that are feasible using current payments.
Consequently, determining adequate payment amounts for primary care practices requires estimating what it would cost for a practice to deliver high-quality care.
The Cost of Delivering Primary Care
Figure 2 shows a hypothetical primary care practice and what it might cost to operate such a practice.
FIGURE 2
Annual Expenses for a
Hypothetical Primary Care Practice
| Type of Expense | Amount |
|---|---|
| Physician | $250,000 |
| Medical Assistant | $38,000 |
| Receptionist | $36,000 |
| Billing | $18,000 |
| Benefits | $48,400 |
| Personnel | $390,400 |
| Rent and Utilities | $40,000 |
| EHR and IT | $6,000 |
| Liability Insurance | $6,000 |
| Supplies and Other | $10,000 |
| Non-Staff Overhead | $62,000 |
| Total Expenses | $452,400 |
- The practice has a single primary care physician. Many rural communities are too small to support more than one physician, so it is desirable to design a payment system that will support solo physician practices as well as larger practices. Moreover, it is reasonable to assume that costs for practices with multiple physicians will be roughly proportional to the number of physicians.44 Although there are some economies of scale for practices with two or more physicians, the savings are limited, and there is also evidence of diseconomies of scale with large practices as well as the potential for higher prices and greater challenges in delivering quality care.45
- The physician employs three people: a full-time medical assistant, a full-time receptionist/office manager, and someone to do billing on a part-time basis. This represents 2.5 FTE staff, which is at the low end of what analyses of primary care practice costs have reported as the average number of staff per FTE physician.46
- The physician is paid $250,000 per year, which is just above the average reported salary of $243,000 for primary care physicians in 2019.47 Other staff are assumed to be paid salaries comparable to national averages for those positions.48 In addition to salaries, the physician and staff are assumed to receive health coverage and other basic benefits.49
- The practice rents office space and it pays for computer equipment, an Electronic Health Record (EHR), malpractice and liability insurance, and office supplies and equipment. The amounts a primary care practice would need to spend on these things can vary significantly depending on the community where it is located and other factors, so the actual costs for an individual practice may be higher or lower than the amounts assumed here. However, since these items represent a small portion of total costs, differences in the costs will have a limited impact on the total cost estimate.
Using these assumptions, the total annual cost of operating the hypothetical primary practice will be about $450,000, slightly less than twice the salary paid to the physician. This is a conservative amount, since analyses typically find that costs other than physician salaries represent 50-60% of practice expenses.50
Revenues Under the Current Payment System
The amount of revenue this hypothetical practice could receive under current fee-for-service payment systems depends heavily on how many patients the practice has, how many and what kinds of services the practice delivers to those patients, what kinds of insurance the patients have, and how much each insurer pays for each service. For simplicity, it will be assumed that the primary care physician does not perform any procedures, that no new patients use the practice during the year (so visits are only made by “established patients”)51, and that no patients are seen in hospitals or other settings.52 Moreover, it will be assumed that the primary care practice is paid Medicare rates for services to all patients.
FIGURE 3
Revenues and Expenses
for the Hypothetical
Primary Care Practice
| Physician Time | |
| Weeks Worked Per Year | 50 |
| Hours Worked Per Day | 9.5 |
| Administrative Time | -0.5 |
| Hours for Patient Care | 9.0 |
| Hours for Previous Visit Follow-Up | -1.8 |
| Hours for Patient Visits | 7.2 |
| Visit Revenue | |
| Visits Per Hour | 2 |
| Unfilled Slots Per Day | 1 |
| Total Visits Per Day | 13 |
| Total Visits Per Year | 3,250 |
| Payment Per Office Visit | $87 |
| Total Revenue | $284,253 |
| Total Expenses | $452,400 |
| Profit/Loss | ($168,147) |
While primary care physicians spend the majority of their day seeing patients, a significant proportion of the day is spent on follow-up tasks related to previous visits, such as reviewing the results of lab tests and imaging studies, communicating those results to the patient, communicating with other physicians about referrals, renewing and modifying prescriptions, etc.53 Studies indicate that about 75-85% of the patient care time during the day is spent on (new) visits and the remainder is spent on the follow-up activities from previous visits.54 It is important to distinguish how much time is available for visits and how much time must be spent on the follow-up tasks because there is no direct compensation for the follow-up time; in standard fee-for-service payment systems, the payment for a visit is assumed to cover both the time the physician spends during the visit as well as the time spent on follow-up activities.
Because of this, if the physician spends 9 hours per day on patient care activities55, only about 7 of those hours (80%) will be available for new visits with patients. If the physician sees an average of two patients per hour, the physician would be able to see an average of 14 patients per day. In order to schedule same-day/next-day visits with patients who need them, the physician would need to have open slots on the schedule each day, so it will be assumed that there would only be 13 visits on most days.56
If an average of two patients per hour are being seen, the average visit would last 30 minutes or less; these would typically be classified as either “Level 3” or “Level 4” office visits.57 Assuming a mix of the two types of visits, the average Medicare payment per visit would likely be about $87.58
Figure 3 shows that with these assumptions, the physician practice would receive far less revenue than necessary to cover its costs. If the physician worked 50 weeks per year, seeing an average of 13 patients per day would generate a total of 3,250 visits over the course of the year, and with an average payment of $87, the total revenue would be only $284,000, compared to the total practice expenses of $450,000.
Why Visits Are Short and Physicians Burn Out
There are five possible ways to eliminate this shortfall:
FIGURE 4
More Patient Visits and
Shorter Visit Times
at the Hypothetical
Primary Care Practice
| Physician Time | |
| Weeks Worked Per Year | 50 |
| Hours Worked Per Day | 10.5 |
| Administrative Time | -0.5 |
| Hours for Patient Care | 10.0 |
| Hours for Previous Visit Follow-Up | -2.0 |
| Hours for Patient Visits | 8.0 |
| Visit Revenue | |
| Visits Per Hour | 3 |
| Unfilled Slots Per Day | 1 |
| Total Visits Per Day | 23 |
| Total Visits Per Year | 5,750 |
| Payment Per Office Visit | $80 |
| Total Revenue | $457,574 |
| Total Expenses | $452,400 |
| Profit/Loss | $5,174 |
- The practice could ask to be paid more for each visit.
- The practice could look for ways to cuts its costs. The biggest costs are personnel costs and office space, but:
- without a full-time receptionist, the practice would likely be unable to schedule as many visits;
- without a medical assistant to help with patient care and follow-up, the physician would have to spend more time in visits and be unable to see as many patients;
- without billing services, the practice would likely not be paid properly for many of its visits;
- lower-cost office space, if available, might not be in a location as convenient or safe for patients, which could result in fewer patients and fewer visits.
- The physician could work longer hours so that more time during the day can be spent seeing patients.
- The physician could see patients for shorter amounts of time, thereby allowing more visits during the day.
- The physician could accept a much lower salary.
For most primary care practices, the only realistic solution has been for the primary care physician to work longer hours and to see more patients in shorter visits.
Figure 4 shows that if the physician spends 10 hours per day on patient care activities and sees 3 patients per hour instead of 2, revenue would increase sufficiently to cover the cost of the practice without any reduction in the physician’s salary.59 The physician would still be making a salary lower than most specialists and would be working even longer hours for it.
Seeing three patients per hour does not mean the physician would be spending 20 minutes with each patient. In addition to time spent examining and talking with the patient, the physician needs to document the visit in the medical record, order tests and medications, etc., so the average time spent with the patient would likely be less than 15 minutes.60
Why the Quality of Care is Poor
A primary care practice with this many visits per year will likely need to provide care for about 2,500 total patients, assuming the patients are “average” overall in terms of ages and health status.61 In fact, 2,500 patients is the number that has frequently been used to describe the “standard” size of a primary care practice.62
It is unlikely that this practice could provide good quality care to this many patients. Good quality care means that in addition to addressing acute care needs, the practice would be delivering all appropriate preventive care to the patients and also appropriate care for any chronic conditions they have. It takes time to provide good quality care, and if physicians don’t have the time, patients won’t receive the care they need.63
Two studies estimated how much time a primary care physician would need to spend in order to deliver quality preventive care services and chronic condition management to an average group of patients in addition to acute care services:
- Preventive care was estimated to require an average of 0.71 hours per year per patient if the patients had an age/sex distribution similar to the U.S. population.64
- Care for chronic conditions was estimated to require an average of 0.99 hours per year per patient, assuming typical rates of chronic disease prevalence.65
Another study found that approximately half of visits to a primary care practice are for acute issues, and that the average length of the visits was only 17 minutes.66 If one assumes that on average, patients visit the primary care practice 1.25 times per year for new acute issues (and other visits are for preventive care or issues related to chronic conditions), and that good care for new acute issues would require an average of at least 30 minutes (0.5 hours), acute care visits would require an average of 0.63 hours per year per patient.
For 2,500 patients, all three of these activities – preventive care, chronic condition care, and acute care – would add up to over 5,800 hours per year, or an average of 23 hours per day for the single physician who is supposed to be providing this care.
Some of the preventive care and chronic condition management activities could be safely and appropriately delegated to a nurse and some could be delegated to a medical assistant, which would reduce the total time required by the physician to deliver quality care. One study estimated that 50-77% of the time needed for preventive care could be delegated and 25-47% of the time needed for chronic condition management could be delegated.67 This would require the primary care physician to employ a nurse as well as a medical assistant, which would increase the cost of operating the practice. However, as shown in Figure 5, even if a nurse was available and appropriate tasks were delegated, the physician would still need to spend an average of 15 hours per day on the activities he or she needed to perform themself.
FIGURE 5
Estimated Time Needed to Provide High-Quality Primary Care
| Patients Per Physician |
% of Total Patients |
Visits Per Patient |
Average Hours Per Patient |
Hours Per Patient Per Year |
% Delegated to RN/MA |
Average Hours Per Physician Per Day |
|
|---|---|---|---|---|---|---|---|
| 2,500 | |||||||
| Preventive Care | 100% | 0.71 | 60% | 2.8 | |||
| Acute Care | 100% | 1.25 | 0.50 | 0.63 | 0% | 6.3 | |
| Chronic Care | 40% | 2.48 | 0.99 | 40% | 6.0 | ||
| Total | 15.0 |
Moreover, these time estimates do not include the time needed to consult and apply clinical practice guidelines/SCAMPs for each patient and to utilize a SAINT for patient feedback. If one assumes that the physician would spend: (1) at least five minutes each year consulting preventive care guidelines for each patient, (2) at least ten minutes each year consulting chronic condition management guidelines for each patient with a chronic condition, and (3) at least five minutes consulting appropriate guidelines during each acute visit, that would require nearly two additional hours of the physician’s time every day. The practice would also need to incur additional costs so its electronic health record system integrated the information from the guidelines and stored both documentation for deviations and information supplied by the patient.
FIGURE 6
Appropriate Patient Panel Size for a Primary Care Physician
| Patients Per Physician |
% of Total Patients |
Visits Per Patient |
Average Hours Per Patient |
Hours Per Patient Per Year |
% Delegated to RN/MA |
Average Hours Per Physician Per Day |
|
|---|---|---|---|---|---|---|---|
| 1,250 | |||||||
| Preventive Care | 100% | 0.79 | 60% | 1.6 | |||
| Acute Care | 100% | 1.25 | 0.58 | 0.73 | 0% | 3.6 | |
| Chronic Care | 40% | 2.65 | 1.06 | 40% | 3.2 | ||
| Open Slots | 0.5 | ||||||
| Total | 8.9 |
The only way to achieve a reasonable workload for the physician would be for the primary practice to have a smaller number of patients in total. As shown in Figure 6, if the primary care practice spends more time per patient to ensure appropriate use of guidelines and employs a nurse so the physician could delegate a significant portion of the tasks, a physician spending 9 hours per day on patient care could provide quality care to about 1,250 patients in total (assuming an average distribution of ages, gender, and chronic conditions), i.e., half as many as the number the practice is currently assumed to be caring for.
FIGURE 7
Revenues and Expenses for the
Hypothetical Primary Care Practice
With Fewer Patients and a Part-Time Nurse
| Patient Revenues | |
| Total Patients | 1,250 |
| Average Visits Per Patient | 2.3 |
| Total Visits Per Year | 2,875 |
| Payment Per Office Visit | $87 |
| Total Revenue | $250,125 |
| Practice Expenses | |
| Physician | $250,000 |
| Nurse (0.5 FTE) | $40,000 |
| Medical Assistant | $38,000 |
| Receptionist | $36,000 |
| Billing | $18,000 |
| Benefits | $56,400 |
| Rent and Utilities | $45,000 |
| EHR and IT | $10,000 |
| Liability Insurance | $9,000 |
| Supplies and Other | $12,000 |
| Total Expenses | $514,400 |
| Profit/Loss | ($264,275) |
However, this cannot be done under standard fee-for-service payments. Figure 7 shows what would happen if the primary care practice employed a half-time nurse, spent more on its EHR, and reduced the size of its patient panel to 1,250 – the combination of higher costs and lower revenues would result in a loss so large that the physician would be unable to receive any salary at all.
Amounts Needed to Support Quality Care
The amount currently paid per visit would have to be doubled in order to enable the practice in Figure 7 to receive sufficient revenues to cover its costs. However, increasing visit fees would not solve the other problems with fee-for-service payment described earlier, and in some ways, it would exacerbate them. The primary care practice would still only be paid for office visits with the physician, so if the practice helped patients with chronic conditions to manage their conditions successfully and helped other patients to stay healthy, the patients would likely make fewer visits to the practice, reducing its revenue. The larger the amount paid per visit, the bigger the financial penalty if fewer visits are needed.
The key to good primary care is enabling the physician and other practice staff to spend an adequate amount of time providing preventive and wellness care, chronic condition management, and acute care. Section 4-B defined the patient-centered method of paying the primary care practice that does not tie payments for wellness care and chronic condition management to office visits. The time estimates shown in Figure 6 can be used to determine amounts the hypothetical primary care practice would need to receive for each of these payments in order to cover its costs:
- a $7.40 Monthly Wellness Care Management Payment for each of the 1,250 patients would provide enough revenue to pay for the time needed by the physician, nurse, and medical assistant to provide appropriate preventive care to the patients as well as pay for a proportional share of the practice overhead.
- a $30.60 Monthly Chronic Condition Management Payment for each of the 500 patients who have chronic conditions (i.e., 40% of the 1,250 total patients) would provide enough revenue to pay for the time needed by the physician and nurse to provide proactive chronic care management for those patients as well as pay for a proportional share of the practice overhead.
- a $141 Acute Visit Fee, paid each time a patient has a new, non-emergency acute problem, would provide enough revenue to pay for the time needed by the physician to diagnose and treat those patients, as well as pay for a proportional share of the practice overhead. (If the physician required significantly more than 30 minutes to address a specific need, the practice could be paid two of these Acute Care Visit Fees, for a total of $282.)
FIGURE 8
Revenues and Expenses for the
Hypothetical Primary Care Practice
with Patient-Centered Primary Care Payment
| Patient Characteristics | |
| Total Patients | 1,250 |
| % with Chronic Condition | 40% |
| Acute Visits Per Year Per Patient | 1.25 |
| Patient-Centered Primary Care Payments | |
| Wellness Care Per Month | $7.40 |
| Acute Care Visit Fee | $141 |
| Chronic Condition Mgt Per Month | $30.60 |
| Practice Revenue/Expense | |
| Wellness Care Revenue | $111,000 |
| Acute Care Revenue | $220,313 |
| Chronic Care Revenue | $183,600 |
| Total Revenue | $514,913 |
| Practice Expenses | $514,400 |
| Profit/Loss | $513 |
| Physician Hours Per Day | |
| Preventive Care | 1.6 |
| Acute Care | 3.6 |
| Chronic Condition Care | 3.2 |
| Open Slots | 0.5 |
| Total Time | 8.9 |
As shown in Figure 8, if the practice has 1,250 patients, if all of the patients in the practice are enrolled for wellness care, if 40% of the patients have a chronic condition and enroll to receive help from the practice in managing that condition, and if the patients in the practice make an average of 1.25 visits per year for acute conditions, the practice will receive enough revenue to cover its costs, and the primary care physician will be able to work a reasonable number of hours each day.
If the primary care physician is performing procedures on the patients, the practice will receive additional revenues from the payments for those procedures. However, the time spent performing procedures means the physician will have less time available to see patients for acute problems and chronic conditions, so the practice will not be able to have as many patients overall. Whether the practice receives more or less revenue overall will depend on the adequacy of the payments for the procedures it performs.
Adequacy of Payments for Different Types of Patients
Since a large portion of the revenue would be specifically tied to patients with chronic conditions and acute problems, it might seem that a primary care practice would lose money if a higher proportion of its patients were healthy and did not have chronic diseases or multiple acute problems.
However, if a smaller proportion of patients had chronic conditions, the physician would be able to manage more than 1,250 patients in total. Figure 9 shows that if only 10% of the patients had a chronic condition, the physician could manage 1,725 patients while still working a reasonable number of hours every day; the higher revenues for wellness care and acute care from the larger number of patients would be sufficient to offset the smaller number of chronic condition management payments, so the practice would still be able to cover its costs. Conversely, if 70% of the patients had a chronic condition, the physician would only be able to manage about 990 patients, but the higher revenues for chronic condition management would offset the lower revenues for wellness care and acute care.
FIGURE 9
Primary Care Practice Revenues and Expenses
and Physician Workload
Under Patient-Centered Primary Care Payment
With Different Types of Patients
| Patient Characteristics | Fewer Chronic Conditions |
More Chronic Conditions |
More Acute Problems |
|
| Total Patients | 1,250 | 1,725 | 990 | 880 |
| % with Chronic Condition | 40% | 10% | 70% | 40% |
| Acute Visits Per Year Per Patient | 1.25 | 1.25 | 1.25 | 2.50 |
| Patient-Centered Primary Care Payments | ||||
| Wellness Care Per Month | $7.40 | $7.40 | $7.40 | $7.40 |
| Acute Care Visit Fee | $141 | $141 | $141 | $141 |
| Chronic Condition Mgt Per Month | $30.60 | $30.60 | $30.60 | $30.60 |
| Practice Revenue/Expense | ||||
| Wellness Care Revenue | $111,000 | $153,180 | $87,912 | $78,144 |
| Acute Care Revenue | $220,313 | $304,031 | $174,488 | $310,200 |
| Chronic Care Revenue | $183,600 | $63,342 | $254,470 | $129,254 |
| Total Revenue | $514,913 | $520,553 | $516,869 | $517,598 |
| Practice Expenses | $514,400 | $514,400 | $514,400 | $514,400 |
| Profit/Loss | $513 | $6,153 | $2,469 | $3,198 |
| Physician Hours Per Day | ||||
| Preventive Care | 1.6 | 2.2 | 1.3 | 1.1 |
| Acute Care | 3.6 | 5.0 | 2.9 | 5.1 |
| Chronic Condition Care | 3.2 | 1.1 | 4.4 | 2.2 |
| Open Slots | 0.5 | 0.5 | 0.5 | 0.5 |
| Total Time | 8.9 | 8.8 | 9.0 | 9.0 |
Similarly, if the primary care practice happens to have a group of patients that experience acute problems frequently, then in order to address those acute problems in a timely fashion, the practice will need to have fewer patients in total. Because the practice is paid for each acute visit, the revenue from the larger number of visits will offset the loss of monthly revenue caused by having fewer patients. Figure 9 also shows an example in which the patients visit the practice twice as often (2.5 times per year on average); the practice could only manage about 880 patients, but the revenues would still be sufficient to cover the practice’s costs.
This demonstrates that with separate payments for wellness care, acute care, and chronic condition management, the primary care practice’s revenues will be automatically risk-adjusted without having to change the fees for any of the individual components based on the patients’ characteristics. If a higher or lower percentage of a practice’s patients have a chronic condition, the revenue to the practice will increase or decrease in a way that approximately matches the changes in the average cost per patient.
As shown in Figure 10, the primary care practice will need to adjust the number of patients it enrolls for care based on the needs of those patients. If a large percentage of the patients who want to enroll in the practice have chronic diseases, complex conditions, or frequent acute problems, the practice will have to enroll fewer patients in total (per physician) to reflect the larger amount of time per patient that the physician and other practice staff will need to devote to their care. However, the smaller number of patients will not reduce the primary care practice’s revenue because the practice will receive bigger payments for the higher-need patients. Conversely, if the patients who enroll in the practice are relatively healthy, the practice can enroll more patients, and it will need to do so to generate adequate revenue to cover its costs.
FIGURE 10
Differences in Number of Enrolled Patients Based on Differences in Patient Needs
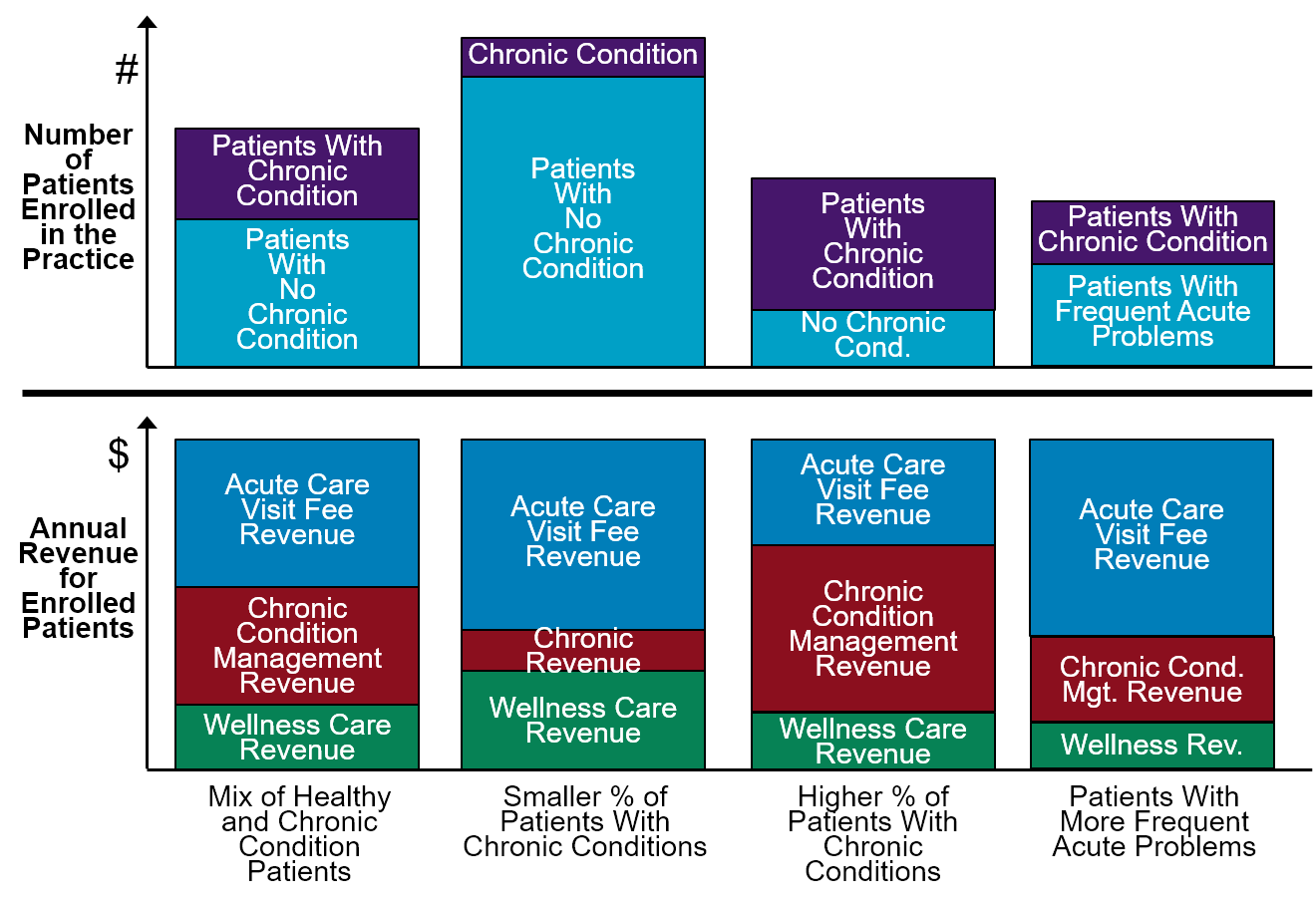
This also means that the payments from a health plan for its members or from an employer for its employees will automatically be adjusted for differences in the number and types of primary care services those members or employees need to receive. Figure 11 shows two different groups of 100 patients. In the first group, 20% of the individuals have a chronic condition and they have acute problems once or twice a year on average. In the second group, it is assumed that the majority of patients have a chronic condition and also that they have acute problems an average of 4 times per year.68 The average monthly amount paid for primary care services to the second group would be more than twice as high as the average monthly payments for the first group, even though the payments for each individual type of service would be exactly the same for every patient, because of the differences assumed in the characteristics of the patients. The health plan for the second group of patients would be spending more because the patients need more services, but it would be paying the same amount for each of those services as every other health plan.
FIGURE 11
Spending on Primary Care For Different Purchasers
| Purchaser A | Purchaser B | |
|---|---|---|
| Total Patients | 100 | 100 |
| % with Chronic Condition | 20% | 60% |
| Acute Visits Per Year Per Patient | 1.25 | 4.00 |
| Wellness Care Per Month | $7.40 | $7.40 |
| Acute Care Visit Fee | $141 | $141 |
| Chronic Condition Mgt Per Month | $30.60 | $30.60 |
| Spending on Primary Care | ||
| Wellness Care Payments | $8,880 | $8,880 |
| Acute Care Payments | $17,625 | $56,400 |
| Chronic Care Payments | $7,344 | $22,032 |
| Total Payments | $33,849 | $87,312 |
| Average Per Member Per Month | $28.21 | $72.76 |
Payment for Integrated Behavioral Health Services
In order to deliver basic integrated behavioral health services in addition to the wellness care, chronic condition management, and acute care services described above, a primary care practice will need to employ or contract with at least one individual who has behavioral health expertise. As discussed in Section 4-B, one option for this is hiring a nurse care manager who receives consulting support from a psychiatrist, and another is a psychologist or a clinical social worker.
For a solo physician practice or even a practice with a small number of physicians, there will likely not be a sufficient number of patients to justify hiring a full-time behavioral health specialist; on the other hand, hiring someone on a part-time basis (assuming someone was available to work on this basis) would not enable providing immediate assistance to patients in conjunction with visits made to the practice. However, since the solo physician practice may also not have enough patients to justify hiring a full-time nurse just for chronic condition management and preventive care support, a solution would be for the small practice to hire a full-time nurse care manager with training in behavioral health management who can play both roles, while larger practices can have separate, more specialized staff if they choose.
FIGURE 12
Revenues and Expenses for the
Hypothetical Primary Care Practice
with Integrated Behavioral Healthcare Services
| Patient Characteristics | |
| Total Patients | 1,250 |
| % with Chronic Condition | 40% |
| Acute Visits Per Year Per Patient | 1.25 |
| Patient-Centered Primary Care Payments | |
| Wellness Care Per Month | $7.40 |
| Behavioral Healthcare Per Month | $4.25 |
| Acute Care Visit Fee | $141 |
| Chronic Condition Mgt Per Month | $30.60 |
| Practice Revenue | |
| Wellness Care Revenue | $111,000 |
| Behavioral Healthcare Revenue | $63,750 |
| Acute Care Revenue | $220,313 |
| Chronic Care Revenue | $183,600 |
| Total Revenue | $578,663 |
| Practice Expenses | |
| Physician | $250,000 |
| Nurse/BH Care Manager | $80,000 |
| Medical Assistant | $38,000 |
| Receptionist | $36,000 |
| Billing | $18,000 |
| Benefits | $64,400 |
| Rent and Utilities | $50,000 |
| EHR and IT | $10,000 |
| Liability Insurance | $12,000 |
| Psychiatric Consultations | $6,250 |
| Supplies and Other | $13,000 |
| Total Expenses | $577,650 |
| Profit/Loss | $1,013 |
As discussed in Section 4-B, the cost of the core behavioral health services staff should be supported through an additional monthly payment for each patient enrolled in the practice for wellness care, rather than fees based on counseling sessions. To be adequate, the amount of the monthly payment must be large enough such that the total revenue the practice receives from the payments is greater than the cost incurred in employing or contracting for the core behavioral health services staff.
Figure 12 shows a hypothetical primary care practice with one physician that hires a full-time nurse who serves approximately half of the time as a care manager for behavioral health issues (with consulting support from a psychiatrist), and the rest of the time providing care management for patients with chronic conditions and support for general wellness and preventive care for all patients. A monthly payment of $4.25 for each patient enrolled in the practice would be sufficient to cover the additional costs of this service beyond the costs and revenues for the other services described earlier. Overall, the practice would be receiving about $11.65 per month ($7.40 + $4.25) for each patient who is enrolled for wellness care.
Higher Payments for Larger Staff Teams
It may be necessary for some primary care practices to have a larger staff team than what is shown in Figure 12.
- A primary care practice may not be able to hire a nurse who is willing or able to provide both chronic care management and behavioral health services, so two nurses would be needed;
- A higher proportion of patients in the practice may have behavioral health care needs, so a full-time behavioral health care manager would be needed.
It may also be viewed as desirable to have more staff available to deliver additional services; for example:
- For patients with multiple health problems, the physician would benefit from the services of a pharmacist in selecting appropriate medications and coordinating the use of multiple medications.
FIGURE 13
Revenues and Expenses for the
Hypothetical Primary Care Practice
with Additional Staff
| Patient Characteristics | |
| Total Patients | 1,250 |
| % with Chronic Condition | 40% |
| Acute Visits Per Year Per Patient | 1.25 |
| Patient-Centered Primary Care Payments | |
| Wellness Care Per Month | $9.30 |
| Behavioral Healthcare Per Month | $8.00 |
| Acute Care Visit Fee | $146 |
| Chronic Condition Mgt Per Month | $43.10 |
| Practice Revenue | |
| Wellness Care Revenue | $139,500 |
| Behavioral Healthcare Revenue | $120,000 |
| Acute Care Revenue | $228,125 |
| Chronic Care Revenue | $258,600 |
| Total Revenue | $746,225 |
| Practice Expenses | |
| Physician | $250,000 |
| Nurse | $80,000 |
| Behavioral Healthcare Manager | $80,000 |
| Pharmacist (0.25 FTE) | $40,000 |
| Medical Assistant | $38,000 |
| Receptionist | $36,000 |
| Billing | $18,000 |
| Benefits | $88,400 |
| Rent and Utilities | $60,000 |
| EHR and IT | $12,000 |
| Liability Insurance | $15,000 |
| Psychiatric Consultations | $6,250 |
| Supplies and Other | $15,000 |
| Total Expenses | $738,650 |
| Profit/Loss | $7,575 |
Additional staff will increase the cost of operating the primary care practice, and higher amounts of payment will be needed to support that. Figure 13 shows a hypothetical primary care practice with a full-time nurse and a full-time behavioral health care manager, rather than a single individual playing both roles, and with a part-time pharmacist assisting with medication management. The cost of operating this practice would be 28% higher than the practice in Figure 12. Consequently, it would need to receive 28% more revenue than it would receive from the Patient-Centered Primary Care Payment amounts shown in Figure 12.
Since the higher costs would be primarily associated with the practice’s behavioral health and chronic condition management services, it would be appropriate to increase those payment amounts by more than 28%, rather than simply increasing all of the payments proportionally. This would ensure that the revenues from the payments remain proportionate to costs for practices with different mixes of patients and correspondingly different numbers and types of staff. Moreover, it would be desirable to minimize any increase in the Acute Care Visit Fee in order to avoid discouraging patients from seeking help from the primary care practice when they have an acute problem.
Figure 13 shows estimated payment amounts that would provide adequate revenues to support the larger primary care team in a way that would achieve these goals.
Adequacy of Payments For Alternative Staffing Arrangements
The payment amounts calculated above are based on a set of assumptions about the number and mix of staff in the primary care practice and the number and types of patients for whom the practice could deliver high-quality care using those resources. However, the payments do not require that the primary care practice be staffed in that specific way if it delivers care to patients with those characteristics. If the primary care practice is receiving Patient-Centered Primary Care Payment, it would have the flexibility to use different types and numbers of staff depending on the needs of the specific set of patients it was caring for. It would also have the responsibility of ensuring that it did not accept more patients, or more high-need patients, than it could deliver high-quality care to with the number and type of staff that it has.
Figure 14 shows three different hypothetical primary care practices that were described in a 2007 article on primary care payment reform by Goroll, Berenson, Schoenbaum, and Gardner.69 Each of the hypothetical practices has two primary care providers – a physician and either a full time or half-time nurse practitioner. Two of the practices have part-time nutritionists and social workers in addition to a nurse and medical assistant. The staff compensation amounts and other costs shown in Figure 14 are identical to the estimates used in the article.
FIGURE 14
Revenues and Expenses for Three Hypothetical Primary Care Practices
| Patient Characteristics | Practice A | Practice B | Practice C | |||||
| Total Patients | 2,000 | 1,250 | 1,500 | |||||
| % with Chronic Condition | 45% | 80% | 50% | |||||
| Acute Visits Per Year Per Patient | 1.50 | 2.75 | 1.75 | |||||
| Practice Revenue | Payment | Revenue | Revenue | Revenue | ||||
| Wellness Care | $7.40 | $177,600 | $111,000 | $133,200 | ||||
| BH Care Revenue | $4.25 | $102,000 | $63,750 | $0 | ||||
| Acute Care Revenue | $141 | $423,000 | $484,688 | $370,125 | ||||
| Chronic Care Revenue | $30.60 | $330,480 | $367,200 | $275,400 | ||||
| Total Revenue | $1,033,080 | $1,026,638 | $778,725 | |||||
| Practice Expenses | Unit Cost | FTE | Expenses | Expenses | Unit Cost | FTE | Expenses | |
| Physician | $250,000 | 1.0 | $250,000 | $250,000 | $200,000 | 1.0 | $200,000 | |
| Nurse Practitioner | 100,000 | 1.0 | $100,000 | $100,000 | $100,000 | 0.5 | $50,000 | |
| RN | $90,000 | 1.0 | $90,000 | $90,000 | $90,000 | 0.5 | $45,000 | |
| Nutritionist | $70,000 | 0.5 | $35,000 | $35,000 | $70,000 | 0.0 | $0 | |
| Social Worker | $70,000 | 0.5 | $35,000 | $35,000 | $70,000 | 0.0 | $0 | |
| Medical Assistant | $50,000 | 1.0 | $50,000 | $50,000 | $50,000 | 1.0 | $50,000 | |
| Receptionist | $60,000 | 1.0 | $60,000 | $60,000 | $60,000 | 1.0 | $60,000 | |
| Benefits | $90,000 | $90,000 | $80,000 | |||||
| Performance Bonus | $50,000 | 100% | $50,000 | $50,000 | $35,000 | 100% | $35,000 | |
| Rent and Utilities | $40,000 | $40,000 | $40,000 | |||||
| EHR and IT | $100,000 | $100,000 | $90,000 | |||||
| Liability Insurance | $50,000 | $50,000 | $50,000 | |||||
| Supplies and Other | $50,000 | $50,000 | $50,000 | |||||
| Total Expenses | $1,000,000 | $1,000,000 | $750,000 | |||||
| Profit/Loss | Margin | Margin | Margin | |||||
| $33,080 | $26,638 | $28,725 | ||||||
| % Profit/Loss | 3% | 3% | 4% | |||||
| Cost Per Patient Per Year | $500 | $800 | $500 | |||||
| Provider Time Per Day | Hours | Hours | Hours | |||||
| Preventive Care | 1.3 | 0.8 | 1.3 | |||||
| Acute Care | 3.5 | 4.0 | 4.1 | |||||
| Chronic Condition Care | 2.9 | 3.2 | 3.2 | |||||
| Open Slots | 1.0 | 1.0 | 0.5 | |||||
| Total Hours Per Day | 8.6 | 9.0 | 9.0 | |||||
| Practice expense estimates based on: Goroll AH, Berenson RA , Schoenbaum SC, Gardner LB. “Fundamental Reform of Payment for Adult Primary Care: Comprehensive Payment for Comprehensive Care” Journal of General Internal Medicine 22:410-415 |
||||||||
Although the article proposes a patient panel size for each practice, it only describes the characteristics of the patients as “low-medium risk” or “medium risk.” In order to estimate the revenue each of these practices would receive under Patient-Centered Primary Care Payment, Figure 14 makes assumptions about the proportion of the patients who have a chronic condition and the number of acute visits the patients would make during the year. The assumptions are chosen such that each provider would be estimated to spend about 8.5 to 9.0 hours per day delivering patient care. Moreover, because the third practice does not have any staff specifically identified that could provide behavioral health support, it is assumed that it would not qualify for the monthly payments for Behavioral Health Services.
Using these assumptions, Figure 14 shows that with the Patient-Centered Primary Care Payment amounts estimated earlier, each of the three hypothetical practices would receive more than enough revenue to cover the estimated cost of operating each practice with its assumed staffing arrangement. If the patients have different characteristics than what is assumed (e.g., a higher or lower proportion of patients with chronic conditions), then the revenue under Patient-Centered Primary Care Payment would be different, but the practice would also need to adjust the size of the patient panel accordingly. For example, as shown in Figure 15, if only 40% of the patients in the first hypothetical practice had a chronic condition instead of 45% and if the patients overall had fewer acute visits per year on average, then the physician and nurse practitioner should have enough time available to manage 2,250 patients in total (an average of 1,125 patients each for the physician and nurse practitioner) instead of only 2,000 patients, and the practice would still receive enough revenue through Patient-Centered Primary Care Payment to cover its costs.
FIGURE 15
Revenues and Expenses for a Hypothetical Primary Care Practice
With Different Numbers and Types of Patients
| Patient Characteristics | Practice A | Alternative Patient Panel |
||
| Total Patients | 2,000 | 2,250 | ||
| % with Chronic Condition | 45% | 40% | ||
| Acute Visits Per Year Per Patient | 1.50 | 1.25 | ||
| Practice Revenue | Payment | Revenue | Revenue | |
| Wellness Care | $7.40 | $177,600 | $199,800 | |
| BH Care Revenue | $4.25 | $102,000 | $114,750 | |
| Acute Care Revenue | $141 | $423,000 | $396,563 | |
| Chronic Care Revenue | $30.60 | $330,480 | $330,480 | |
| Total Revenue | $1,033,080 | $1,041,593 | ||
| Practice Expenses | Unit Cost | FTE | Expenses | Expenses |
| Physician | $250,000 | 1.0 | $250,000 | $250,000 |
| Nurse Practitioner | 100,000 | 1.0 | $100,000 | $100,000 |
| RN | $90,000 | 1.0 | $90,000 | $90,000 |
| Nutritionist | $70,000 | 0.5 | $35,000 | $35,000 |
| Social Worker | $70,000 | 0.5 | $35,000 | $35,000 |
| Medical Assistant | $50,000 | 1.0 | $50,000 | $50,000 |
| Receptionist | $60,000 | 1.0 | $60,000 | $60,000 |
| Benefits | $90,000 | $90,000 | ||
| Performance Bonus | $50,000 | 100% | $50,000 | $50,000 |
| Rent and Utilities | $40,000 | $40,000 | ||
| EHR and IT | $100,000 | $100,000 | ||
| Liability Insurance | $50,000 | $50,000 | ||
| Supplies and Other | $50,000 | $50,000 | ||
| Total Expenses | $1,000,000 | $1,000,000 | ||
| Profit/Loss | Margin | Margin | ||
| $33,080 | $41,593 | |||
| % Profit/Loss | 3% | 4% | ||
| Cost Per Patient Per Year | $500 | $444 | ||
| Provider Time Per Day | Hours | Hours | ||
| Preventive Care | 1.3 | 1.4 | ||
| Acute Care | 3.5 | 3.3 | ||
| Chronic Condition Care | 2.9 | 2.9 | ||
| Open Slots | 1.0 | 1.0 | ||
| Total Hours Per Day | 8.6 | 8.6 | ||
| Practice expense estimates based on: Goroll AH, Berenson RA , Schoenbaum SC, Gardner LB. “Fundamental Reform of Payment for Adult Primary Care: Comprehensive Payment for Comprehensive Care” Journal of General Internal Medicine 22:410-415 |
||||
The assumptions used in Figure 12 to estimate the appropriate amounts under Patient-Centered Primary Care Payment are also based on a staffing configuration and costs that would be feasible for a small primary care practice with a single physician. Larger practices with multiple physicians, or a combination of physicians and nurse practitioners or physician assistants, could potentially hire other types of staff, such as pharmacists and community health workers. Patient-Centered Primary Care Payment would provide the flexibility for a practice to hire different kinds of staff if it wished to do so, since the payments are not tied to any particular staffing arrangement. However, a practice would only receive enough revenues to do so under Patient-Centered Primary Care Payment if the practice has enough patients with the appropriate needs to make it cost-effective to hire more and different staff.
For example, Figure 16 shows four different staffing configurations and costs for primary care practices that were proposed in a 2018 article by Meyers and colleagues.70 Although the article described some of the characteristics of the patients assumed to be in each practice, there was not enough information to calculate the amount of revenues that the practices would receive under Patient-Centered Primary Care Payment, so Figure 16 makes some additional assumptions about the average number of acute visits per year the patients in each practice would make and about the number of chronic conditions the patients have in the third and fourth practices.
FIGURE 16
Revenues and Expenses for Four Hypothetical Primary Care Practices
| Patient Characteristics | Index Model |
High Geriatric Model |
High Social Need Model |
Rural Model |
|||||
| Total Patients | 10,000 | 10,000 | 10,000 | 5,000 | |||||
| % with Chronic Condition | 32% | 65% | 40% | 45% | |||||
| Acute Visits Per Year Per Patient | 1.25 | 2.75 | 2.75 | 1.50 | |||||
| Practice Revenue | Payment | Revenue | Revenue | Revenue | Revenue | ||||
| Wellness Care | $7.40 | $888,000 | $888,000 | $888,000 | $444,000 | ||||
| BH Care Revenue | $4.25 | $510,000 | $510,000 | $510,000 | $255,000 | ||||
| Acute Care Revenue | $141 | $1,762,500 | $3,877,500 | $3,877,500 | $1,057,500 | ||||
| Chronic Care Revenue | $30.60 | $1,175,040 | $2,386,800 | $1,468,800 | $826,200 | ||||
| Total Revenue | $4,335,540 | $7,662,300 | $6,744,300 | $2,582,700 | |||||
| Practice Expenses | Unit Cost | FTE | Expenses | FTE | Expenses | FTE | Expenses | FTE | Expenses |
| Physician | $235,512 | 6.3 | $1,597,126 | 8.3 | $2,104,150 | 5.3 | $1,343,614 | 2.2 | $557,726 |
| Nurse Practitioner | $127,251 | 2.0 | $254,502 | 4.0 | $509,004 | 5.0 | $636,255 | 2.0 | $254,502 |
| RN | $80,568 | 4.5 | $362,556 | 7.0 | $563,976 | 7.0 | $563,976 | 1.8 | $145,022 |
| LPN | $51,677 | 0.5 | $25,839 | 0.0 | $0 | 0.0 | $0 | 1.0 | $51,677 |
| Social Worker | $83,048 | 1.5 | $124,572 | 3.0 | $249,144 | 2.0 | $166,096 | 1.8 | $145,334 |
| Therapist | $64,129 | 1.0 | $64,129 | 0.0 | $0 | 0.0 | $0 | 0.0 | $0 |
| Psychologist | $95,935 | 0.0 | $0 | 0.0 | $0 | 1.0 | $95,935 | 0.0 | $0 |
| Substance Use Counselor | $64,129 | 0.0 | $0 | 0.0 | $0 | 1.0 | $64,129 | 0.0 | $0 |
| Pharmacist | $159,262 | 1.0 | $159,262 | 1.0 | $159,262 | 1.0 | $159,262 | 0.5 | $79,631 |
| Pharmacy Assistant | $49,358 | 0.0 | $0 | 1.0 | $49,358 | 1.0 | $49,358 | 0.0 | $0 |
| Medical Assistant | $40,841 | 11.0 | $449,251 | 15.0 | $612,615 | 13.0 | $530,933 | 8.0 | $326,728 |
| Community Health Worker | $46,470 | 1.0 | $46,470 | 1.0 | $46,470 | 2.0 | $92,940 | 1.0 | $46,470 |
| Patient Navigator | $49,177 | 0.0 | $0 | 1.0 | $49,177 | 2.0 | $98,354 | 0.0 | $0 |
| Receptionist | $41,589 | 8.0 | $332,712 | 11.0 | $457,479 | 10.0 | $415,890 | 4.0 | $166,356 |
| General Operating Cost | $1,767,000 | $2,651,000 | $2,209,000 | $884,000 | |||||
| Business Operating Cost | $188,000 | $282,000 | $235,000 | $94,000 | |||||
| Total Expenses | $5,371,418 | $7,733,635 | $6,660,742 | $2,751,447 | |||||
| Profit/Loss | ($1,035,878) | ($71,335) | $83,558 | ($168,747) | |||||
| % Profit/Loss | -19% | -1% | 1% | -6% | |||||
| Cost Per Patient Per Year | $537 | $773 | $666 | $550 | |||||
| Number of Providers | 8.3 | 12.3 | 10.3 | 4.2 | |||||
| Cost Per Provider | $647,159 | $628,751 | $646,674 | $655,106 | |||||
| Provider Time Per Day | Hours | Hours | Hours | Hours | |||||
| Preventive Care | 1.5 | 1.0 | 1.2 | 1.5 | |||||
| Acute Care | 3.5 | 5.2 | 6.2 | 4.2 | |||||
| Chronic Condition Care | 2.4 | 3.4 | 2.5 | 3.4 | |||||
| Open Slots | 0.5 | 0.5 | 0.5 | 0.5 | |||||
| Total Hours Per Day | 8.0 | 10.1 | 10.4 | 9.6 | |||||
| Practice expense estimates based on: Meyers D et al. “Workforce Configurations to Provide High-Quality Comprehensive Primary Care: A Mixed-Method Exploration of Staffing for Four Types of Primary Care Practices.” *Journal of General Internal Medicine* 33(10):1774-1779 |
|||||||||
Figure 16 shows that the second and third practices would roughly break even if they received the Patient-Centered Primary Care Payment amounts estimated earlier, but the first and fourth practices would not. This does not mean that the Patient-Centered Primary Care Payment amounts are too low, but rather that the first and fourth practices likely have more staff and higher costs than necessary to deliver high-quality care to the number and types of patients they are assumed to have. In the hypothetical single-physician practice in Figure 12 that was used to estimate adequate amounts for Patient-Centered Primary Care Payment, the practice had 3.5 staff in addition to the physician, and total practice expenses of $578,000. In contrast, for the practices shown in Figure 16, there are between 3.4 and 4.3 staff per provider and the average expense per provider is about $650,000. The higher cost per primary care provider is the primary reason the first practice in Figure 16 would experience a loss under the estimated Patient-Centered Primary Care Payment amounts. The other reason is that fewer patients in the first practice have chronic diseases and the primary care physicians and nurse practitioners also have fewer patients on average than were assumed in Figure 12.
Figure 17 shows that if the first practice in Figure 16 had additional patients and fewer staff and costs, such that the provider workload and the staff and costs per provider were more in line with the assumptions in Figure 12, it would also be able to cover its costs using the Patient-Centered Primary Care Payment amounts. Conversely, if the patients in the practice or those paying for their care felt it was desirable for the practice to have additional staff and lower provider workloads, they would need to pay higher amounts for the practice’s services in order to support that. As shown in the third column of Figure 17, the higher payment amounts that were estimated in Figure 13 for supporting a larger primary care team would be sufficient to cover the costs of this practice.
FIGURE 17
Revenues and Expenses for a Hypothetical Primary Care Practice
With Different Patients, Staffing, and Revenues
| Patient Characteristics | Index Model (Figure 16) |
More Patients and Fewer Staff |
Higher Payments |
||||
| Total Patients | 10,000 | 11,250 | 10,000 | ||||
| % with Chronic Condition | 32% | 32% | 32% | ||||
| Acute Visits Per Year Per Patient | 1.25 | 1.25 | 1.25 | ||||
| Practice Revenue | Payment | Revenue | Revenue | Payment | Revenue | ||
| Wellness Care | $7.40 | $888,000 | $999,000 | $9.30 | $1,116,000 | ||
| BH Care Revenue | $4.25 | $510,000 | $573,750 | $8.00 | $960,000 | ||
| Acute Care Revenue | $141 | $1,762,500 | $1,982,813 | $146 | $1,825,000 | ||
| Chronic Care Revenue | $30.60 | $1,175,040 | $1,321,920 | $43.10 | $960,000 | ||
| Total Revenue | $4,335,540 | $4,877,483 | $5,556,040 | ||||
| Practice Expenses | Unit Cost | FTE | Expenses | FTE | Expenses | FTE | Expenses |
| Physician | $235,512 | 6.3 | $1,597,126 | 6.3 | $1,597,126 | 6.3 | $1,597,126 |
| Nurse Practitioner | $127,251 | 2.0 | $254,502 | 2.0 | $254,502 | 2.0 | $254,502 |
| RN | $80,568 | 4.5 | $362,556 | 4.5 | $362,556 | 4.5 | $362,556 |
| LPN | $51,677 | 0.5 | $25,839 | 0.5 | $25,839 | 0.5 | $25,839 |
| Social Worker | $83,048 | 1.5 | $124,572 | 1.5 | $124,572 | 1.5 | $124,572 |
| Therapist | $64,129 | 1.0 | $64,129 | 1.0 | $64,129 | 1.0 | $64,129 |
| Psychologist | $95,935 | 0.0 | $0 | 0.0 | $0 | 0.0 | $0 |
| Substance Use Counselor | $64,129 | 0.0 | $0 | 0.0 | $0 | 0.0 | $0 |
| Pharmacist | $159,262 | 1.0 | $159,262 | 0.0 | $0 | 1.0 | $159,262 |
| Pharmacy Assistant | $49,358 | 0.0 | $0 | 0.0 | $0 | 0.0 | $0 |
| Medical Assistant | $40,841 | 11.0 | $449,251 | 8.0 | $326,728 | 11.0 | $449,251 |
| Community Health Worker | $46,470 | 1.0 | $46,470 | 1.0 | $46,470 | 1.0 | $46,470 |
| Patient Navigator | $49,177 | 0.0 | $0 | 0.0 | $0 | 0.0 | $0 |
| Receptionist | $41,589 | 8.0 | $332,712 | 8.0 | $332,712 | 8.0 | $332,712 |
| General Operating Cost | $1,767,000 | $1,501,950 | $1,767,000 | ||||
| Business Operating Cost | $188,000 | $188,000 | $188,000 | ||||
| Total Expenses | $5,371,418 | $4,824,583 | $5,371,418 | ||||
| Profit/Loss | ($1,035,878) | $52,899 | $184,622 | ||||
| % Profit/Loss | -19% | +1% | +3% | ||||
| Cost Per Patient Per Year | $537 | $429 | $537 | ||||
| Number of Providers | 8.3 | 8.3 | 8.3 | ||||
| Cost Per Provider | $647,159 | $581,275 | $647,159 | ||||
| Provider Time Per Day | Hours | Hours | Hours | ||||
| Preventive Care | 1.5 | 1.7 | 1.5 | ||||
| Acute Care | 3.5 | 4.0 | 3.5 | ||||
| Chronic Condition Care | 2.4 | 2.8 | 2.4 | ||||
| Open Slots | 0.5 | 0.5 | 0.5 | ||||
| Total Hours Per Day | 8.0 | 8.9 | 8.0 | ||||
| Index Model practice expense estimates based on: Meyers D et al. “Workforce Configurations to Provide High-Quality Comprehensive Primary Care: A Mixed-Method Exploration of Staffing for Four Types of Primary Care Practices.” *Journal of General Internal Medicine* 33(10):1774-1779 |
|||||||
In contrast, although the staffing and cost ratios are higher for the second and third practices in Figure 16, this is likely justified given that more of the patients in these practices are assumed to have chronic diseases and social challenges that would benefit from additional time and assistance from nurses, social workers, community health workers, etc. as well as adequate time with a physician or other provider. As shown in Figure 16, the amounts estimated for Patient-Centered Primary Care Payment in Figure 12 would provide both adequate revenue and flexibility to do so.
Refining Payment Amounts Over Time
As shown above, calculating adequate payment amounts requires making assumptions about (1) the average amount of time physicians and other primary care providers will need to spend with patients based on the characteristics of those patients, (2) the number and types of staff needed to complement the work of the physicians, (3) the amounts of compensation for each of the staff, and (4) the cost of the equipment and space they need to carry out their work. There are only limited data available today with which to make these assumptions, and there is even less evidence about which types of staffing and approaches to care delivery are necessary for delivering high-quality primary care vs. merely desirable.
However, it is impossible to obtain better data or evidence today, because current payment systems do not allow primary care practices to deliver the desired level of care needed to obtain the data or evidence. Moreover, as will be discussed in Section 5, most primary care payment demonstration projects also do not provide adequate funding or flexibility to generate the data and evidence needed to accurately determine adequate payment amounts for Patient-Centered Primary Care Payment.
The only way to resolve this “chicken and egg” problem is to begin using payment amounts based on best estimates of time and costs (accepting the reality that those amounts may not be exactly “right”), allow primary care practices to use the payments to restructure and improve primary care delivery, gather data on how much time is actually needed to deliver high-quality care, and then refine the amounts over time as those data become available. This process will likely take several years to complete. This is similar to what is done in the current fee-for-service payment system. Each year, CMS adjusts the Medicare payment amounts for various physician services based on new information and evidence about the cost of delivering the services to patients.
Stratifying Wellness and Chronic Condition Payments
This evolutionary approach to setting appropriate payment amounts will be particularly important for determining how much higher the monthly chronic condition management payments should be for patients who have complex conditions or face barriers in obtaining care in standard ways, and how much higher the wellness care payments should be for patients discharged from the hospital or recovering from an illness. There is relatively little information available about the differences in the amounts of time a primary care practice needs to spend with different types of patients in order to provide the services needed to achieve good outcomes71, so in order to set initial payment amounts for different types of patients, assumptions will need to be made about how many patients would be eligible for a higher payment and the differences in time and costs involved in caring for those patients. Both the criteria for paying different amounts and the actual amounts of the payments can be refined based on additional data collected after the initial payments allow primary care practices to begin delivering higher-quality services to these patients.
As a starting point, if it is assumed that about 20% of the patients with chronic conditions have complex conditions that require significantly more time and attention, and if it is assumed that each of those patients requires, on average, twice as much time from the primary care physician and other practice staff as the chronic condition patients who do not have a complex condition, the standard payment for Chronic Condition Management could be set at $24.60 per month and the payment for the complex condition patients could be set at $54.60 per month, as shown in Figure 18.
FIGURE 18
Initial Estimates of Stratified Chronic Condition Management Payments
| Patients Per Physician |
% of Total Patients |
Hours Per Patient |
Hours Per Total Patient Per Year |
% Delegated to RN/MA |
Physician Hours Per Day |
Staff Hours Per Day |
Monthly Payment Per Patient |
|
|---|---|---|---|---|---|---|---|---|
| 1,250 | ||||||||
| Chronic Care | 40% | 2.65 | 1.06 | 40% | 3.2 | 2.1 | $30.60 | |
| Non-Complex | 80% | 2.17 | 0.69 | 42% | 2.5 | 1.8 | $24.60 | |
| Complex | 20% | 4.33 | 0.35 | 30% | 6.1 | 2.6 | $54.60 | |
| Total | 100% | 2.65 | 1.06 | 40% | 3.2 | 2.1 | $30.60 | |
| Cost Per Hour | $187 | $62 | ||||||
If primary care practices receive these amounts for each subgroup, a practice with an “average” group of patients with chronic conditions would still be receiving about $30.60 per month on average for those patients with chronic conditions, but a practice with more complex patients would be receiving higher average payments to reflect the greater time they need to spend providing care to those patients. Practices with a higher number of complex patients would need to have fewer patients in total in order to spend adequate time on those patients, and the higher payments would automatically provide higher revenue to compensate for that.
The higher payment amount for a patient with a newly-diagnosed or newly-treated chronic condition could initially be set at the same amount as for the complex condition patients. Once additional data are available on the differences in time and costs for these patients, both the amount and the length of time during which the higher amount is paid could be revised.
A similar approach could be used to set the higher Wellness Care Payment for the month following a hospitalization or serious illness. If it is assumed that on average, approximately twice as much time as usual would be needed to provide proactive assistance to the patient during this month, then the monthly payment could be set at $14.80 rather than $7.40. Here again, once additional data are available on the additional amount of time needed for these patients, the amount of payment could be revised accordingly.
Payments for Procedures and Tests
Primary care physicians are trained to perform a variety of procedures, such as removing skin lesions, suturing minor wounds, and injecting medications into joints. For many patients, it would be both appropriate and desirable to obtain these procedures from their PCP rather than a specialist, outpatient clinic, or emergency department.
Since these procedures would continue to be paid for on a fee-for-service basis, patients and payers could initially pay primary care practices the same amounts for these services as they pay today. Information could then be gathered from primary care practices to determine whether any of these amounts are inadequate to cover the time and out-of-pocket costs required for the procedures; if so, those payments can be increased appropriately.
It would also be desirable for patients to receive basic laboratory tests at the primary care practice rather than having to go to a hospital or separate laboratory. There are fees currently available for all of these tests, but some of the fees may not be adequate to cover the costs of the equipment and supplies with the volume of tests the primary care practice would perform, particularly in a small primary care practice.
Information should be gathered from primary care practices to determine the average cost of providing common tests that would be desirable to perform on site, and if those costs are higher than current fees, higher fees should be paid to practices participating in the Patient-Centered Primary Care Payment system. Because the primary care practice would be following clinical practice guidelines in ordering tests and the payments would be based on the estimated costs of performing the tests, there should not be any concern about the tests being overused if the payments are increased.
Payments for New Patients
Similarly, the current fee-for-service payment amounts would continue to be used for new patients, and information can be gathered from primary care practices to determine whether any of these amounts are inadequate to cover the time and out-of-pocket costs required for diagnosis and treatment planning for new patients; if so, those payments can be increased appropriately.
Adjustments for Geographic Differences in Costs
If a primary care practice is located in a community where the costs of operating the practice are significantly higher, then the payment amounts for each service would also need to be higher. For example, if the cost of office space is high in a particular area due to high taxes, limited office space, or other factors, or if salaries for medical assistants or nurses have to be higher to attract and retain them in a rural or inner-city area, then the primary care practice will need to be paid more to cover those costs.72
Eliminating Unnecessary Administrative Burdens
One thing that is implicitly assumed in making the estimates of the payment amounts above is that the primary care practice would not be spending any significant amount of time submitting quality measures or prior authorization requests to health insurance companies73, participating in burdensome accreditation processes in order to qualify for adequate payments74, or spending large amounts of time on other administrative requirements imposed by a payer. Because the accountability component in Patient-Centered Primary Care Payment will be more effective in ensuring that patients receive appropriate, high-quality care than quality measures, prior authorization, or accreditation, there would be no need to impose these requirements on the practice.
If a health plan tries to impose these types of administrative burdens on a primary care practice, the practice would have to incur additional costs.75 If the primary care practice was willing to take on these unnecessary administrative burdens in order to continue providing primary care to members of that health plan, the health plan would need to pay the practice more to enable the practice to carry out these tasks, either by increasing the payment amounts for individual services or allowing the practice to bill directly for the time it spends on these activities. However, if the patients have the ability to switch to other types of insurance, the practice could also simply stop accepting insurance from that health plan.
Affordability for Patients
The fourth essential characteristic of a Patient-Centered Primary Care Payment system is that it is affordable for patients. The payments defined above would only generate adequate revenue to cover the primary care practice’s costs if patients actually enroll in the primary care practice and use its services, and patients will be unlikely to do that if they cannot afford the services or if the patients feel that services from a hospital emergency department or another healthcare provider would provide similar benefits at a lower cost.
The affordability of any health service for an individual patient depends on many factors, but one of the most important considerations is whether the patient is paying entirely out of pocket or if they have insurance that covers most of the cost.
Self-Pay Patients
Patients who have no insurance will have to pay the full amount for any services they receive from a primary care practice. In addition, patients on many high-deductible health plans also have to pay the full amount for primary care visits except for required preventive care services.
For these patients, three features of Patient-Centered Primary Care Payment will help make high-quality primary care services as affordable as possible:
- separate payments for wellness care, acute care, and chronic condition management ensure that the patient is not paying for services they do not need or want;
- the payments for wellness care and chronic condition management are spread out over the course of the year, rather than requiring large, lump sum payments when a visit is needed; and
- the payment amounts are based on the cost of delivering high-quality care in an efficient way.
For self-pay patients, the payment amounts defined above would make primary care services as or more affordable than the alternatives available:
- For patients with an acute problem, the $141 payment for the primary care physician to diagnose and treat the condition would be roughly equivalent to what the patient would pay for a visit to an urgent care center, and significantly less than what they would typically have to pay for an emergency department visit;
- Monthly payments of $7.40 for wellness care would total $89 over the course of the year. This amount would be less than the fee the patient would likely have to pay for a single office visit today, and would enable patients to receive advice and assistance over the course of the year rather than just in one short visit.
- A monthly payment of $30.60 for chronic condition management would total $367 over the course of the year ($1 per day). This is a large amount, so it could deter some patients from participating, although even with the wellness care payment, it would be less than the cost of a typical cable TV or cellular phone bill. Patients with a chronic condition will need to understand that without regular, proactive assistance from the primary care practice, they might need to make multiple visits to either the primary care physician, a specialist, or an emergency department during the course of the year, and paying separate amounts for each of these visits could cost the patient more than the monthly payments.
Moreover, the patient would not be charged any fee for a visit, for a month of wellness care, or for a month of chronic condition management if the patient did not receive the appropriate evidence-based services they needed during the visit or during the month. No similar assurance of quality is available from any alternative source of care.
Patients With Insurance Coverage
The issues are different for patients who have a health insurance plan that either (1) does not have a high deductible or (2) covers a portion of primary care visits regardless of whether the deductible has been met. For these patients, it will be important to establish co-payment and coinsurance amounts that make primary care services affordable, both in absolute terms and relative to the cost-sharing amounts required for alternative services. Specifically:
- A Modest Co-payment for Acute Care Visits. A copayment should be required for an Acute Care Visit Fee in order to ensure that some patients do not make visits to the practice for trivial issues. However, the copayment amount should be low enough that patients do not avoid contacting the practice when they have an acute issue that should receive attention. Moreover, the copayment for a primary care visit should be significantly less than the copayment or coinsurance required for an urgent care visit or an emergency department visit; it would be preferable for the patient to receive non-emergency acute care from the primary care practice since the physician’s familiarity with the patient will enable diagnosis and appropriate treatment without ordering unnecessary tests or other services. For example, a copayment of $25-$30 would represent about 20% of the full payment amount, which is a cost-sharing amount similar to what is required in Medicare and many health insurance plans.
- No Cost-Sharing for Wellness Care. No patient cost-sharing should be required for the monthly Wellness Care Payments, nor should they be subject to any deductible. Health insurance plans are not permitted to charge patients for recommended preventive care services, and even though a patient might not be receiving any recommended preventive services during a particular month, it would be simpler and better to simply avoid any cost-sharing for these payments.
- No Cost-Sharing for Chronic Condition Management. Ideally, there would also be no copayments or coinsurance for the monthly Chronic Condition Management Payments, nor would they be subject to a deductible. The goal of these services is to prevent chronic condition exacerbations from occurring, and since the savings to the health plan from not having to pay for hospital treatment of exacerbations will likely exceed the cost of the monthly condition management services, it would be undesirable to create cost barriers that could discourage patients from enrolling to receive these services.76
Summary
Figure 19 summarizes all of the elements of Patient-Centered Primary Care Payment. Although there are multiple separate payments targeted at different subsets of services and different types of patients, all of the payments are necessary to give a primary care practice adequate resources and flexibility to deliver high-quality care for each individual patient. If only a subset of the payments is implemented, the quality of care for all patients would be reduced, because the primary care practice would not be able to employ the appropriate staff and it could be forced to deliver fewer services than necessary for more patients than it can it effectively manage.
FIGURE 19
Summary of Patient-Centered Primary Care Payment
| Type of Service |
Billing Code | Eligible Patients | Frequency of Payment |
Accountability for Quality |
Estimated Amount |
Patient Share |
|---|---|---|---|---|---|---|
| Wellness and Preventive Care |
XX010 Wellness Care |
A patient who enrolls for proactive wellness care | Monthly | Follow evidence-based preventive care guidelines (CPG/SCAMP) and use a SAINT to monitor patient needs | $7.40 per patient per month | $0 |
| XX011 Transitional Care |
A patient who was hospitalized or had a serious illness | Month after hospital discharge or serious illness | Follow evidence-based guidelines (CPG/SCAMP) and use a SAINT to monitor patient needs | $14.80 for the month (instead of $7.40) |
$0 | |
| XX012 Integrated Behavioral Healthcare |
A patient who enrolls for proactive wellness care if the practice has integrated behavioral health services | Monthly in addition to Wellness Care Payment | Follow evidence-based guidelines (CPG/SCAMP) for behavioral health and use a SAINT to monitor patient needs | $4.25 per patient per month (in addition to $7.40) |
$0 | |
| Non-Emergency Acute Care | XX020 Acute Care Visit |
A patient enrolled for wellness care who experiences a new acute symptom or injury that does not require emergency care | For each new acute event | Diagnosis and treatment plan based on evidence-based guidelines (CPG/SCAMP) for the symptom/condition and use of SAINT to monitor outcomes | $141 per visit ($282 for visit requiring more than 45 minutes) |
$25 |
| Chronic Condition Care |
XX030 Initial Management of a Chronic Condition |
A patient with a newly diagnosed or newly treated chronic disease | Following diagnosis or initial treatment | Follow evidence-based guidelines (CPG/SCAMP) for management of the chronic condition and use a SAINT to monitor patient needs | $54.60 per patient for the initial month | $0 |
| XX031 Chronic Condition Management |
A patient with a chronic condition | Monthly | Follow evidence-based guidelines (CPG/SCAMP) for management of the chronic condition and use a SAINT to monitor patient needs | $24.60 per patient per month after the first month | $0 | |
| XX032 Management of a Complex Condition |
A patient with a complex condition | Monthly | Follow evidence-based guidelines (CPG/SCAMP) for management of the complex condition(s) and use a SAINT to monitor patient needs | $54.60 per patient per month | $0 | |
| Procedures and Tests |
Standard code for procedure or test | A patient receiving a procedure or rest | When procedure or test is performed | Follow evidence-based guidelines in ordering test or performing procedure | Payment based on cost of procedure or test | Amount varies |
| New Patient | 99201-99205 | Any patient | When patient is first seen by physician | Follow evidence-based guidelines in evaluating patient needs | Current fee schedule | Current benefits |
Addressing Non-Participating Payers
The estimated Patient-Centered Primary Care Payment amounts will only be adequate if the primary care practice can receive those payments for every patient who wants to enroll for wellness care and/or chronic condition management services from the practice. If the primary care practice is providing care for an appropriate number of patients (1,250 patients for the hypothetical practice described above), but if the health insurance plans for a subset of those patients are not paying adequate amounts or are only willing to pay for services using standard fee-for-service payments, the practice will end up with a financial loss somewhere in between the scenario shown in Figure 7 and the scenario shown in Figure 12. Since the payment amounts described above were designed to be adequate to support the practice’s costs, not to generate significant profits, and since standard fee-for-service payments would cause significant losses, the practice will lose money overall if the practice still receives standard fee-for-service payments for a subset of its patients.
FIGURE 20
Revenues and Expenses for the
Hypothetical Primary Care Practice
With Non-Participating Payers
| Patient Characteristics | |
| Total Patients | 1,250 |
| % with Chronic Condition | 40% |
| Total Visits Per Year Per Patient | 2.30 |
| Acute Visits Per Year Per Patient | 1.25 |
| Standard Fee-for-Service Payment | |
| % of Patients With Standard FFS | 50% |
| Average Fee Per Visit | $80 |
| Patient-Centered Primary Care Payment | |
| Wellness Care Per Month | $7.40 |
| Behavioral Healthcare Per Month | $4.25 |
| Acute Care Visit Fee | $141 |
| Chronic Condition Mgt Per Month | $30.60 |
| Practice Revenue | |
| FFS Visit Revenue | $114,393 |
| Wellness Care Revenue | $55,500 |
| Behavioral Healthcare Revenue | $31,875 |
| Acute Care Revenue | $110,156 |
| Chronic Care Revenue | $91,800 |
| Total Revenue | $403,725 |
| Practice Expenses | |
| Physician | $250,000 |
| Nurse/BH Care Manager | $80,000 |
| Medical Assistant | $38,000 |
| Receptionist | $36,000 |
| Billing | $18,000 |
| Benefits | $64,400 |
| Rent and Utilities | $50,000 |
| EHR and IT | $10,000 |
| Liability Insurance | $12,000 |
| Psychiatric Consultations | $6,250 |
| Supplies and Other | $13,000 |
| Total Expenses | $577,650 |
| Profit/Loss | ($173,925) |
| -30% | |
For example, as shown in Figure 20, if only half of the patients at the hypothetical practice are being paid for through the Patient-Centered Primary Care Payment system, the practice would only receive 70% of the revenues it needed to cover the costs of providing high-quality care to all of the patients in the practice.
However, primary care physicians being paid under Patient-Centered Primary Care Payment will need to provide care to fewer patients than they try to do under the current payment system, because they will need to spend more time with each patient.77 If only a subset of a practice’s current patients have health plans that are willing to pay using Patient-Centered Primary Care Payment, then the primary care practice could focus on delivering care to those patients.
The primary care practice may not want to stop providing care to patients who are insured by non-participating payers, but every practice must either (1) reduce the size of its patient panel or (2) add one or more additional primary care physicians to the practice, because it cannot provide high-quality care to all of its current patients with the current number of physicians. However, a practice cannot afford to hire an additional physician with the fee amounts paid under the current payment system. Since it will only have the time and resources needed to provide high-quality care to the patients whose insurance plans pay adequately for primary care services, it makes sense for the practice to use the health plan’s payment system as one criterion in deciding which patients to continue providing care for. In fact, it would be unfair to the patients whose insurance plans are paying appropriately to have the primary care practice devote less time and effort to their care because the practice is also trying to provide care to patients whose insurance plans are significantly underpaying for care. The primary care practice could decide to stop contracting with a non-participating insurance plan altogether, or it could decide to continue contracting for a period of time but to accept only a small number of patients with that type of insurance.
This is essentially what physicians who form Direct Primary Care practices have been doing.78 The physicians know that they cannot deliver good care to as many patients as they have to see to be paid adequately under the current payment system, so they limit their practice to patients who are willing and able to pay an adequate amount. These physicians do not accept insurance, both because most insurance plans do not pay adequately and appropriately for primary care services and because of the unnecessary administrative burdens most health insurance companies impose for the payments they do make. Under Patient-Centered Primary Care Payment, however, the payments would be adequate and appropriate and there would be no unnecessary administrative burdens, so these physicians could continue to care for patients who have insurance as well as those who can afford to pay without using insurance.
Since different primary care practices have different types of patients with different types of insurance, practices will differ in their ability to only treat patients whose insurance plans use Patient-Centered Primary Care Payment, at least in the short run. If a primary care practice currently has 2,500 patients with an average mix of health problems, and it needs to move to a 1,250-patient panel in order to provide high-quality care, then on average, only half of the health insurance plans for the current patients would need to be using Patient-Centered Primary Care Payment in order for the practice to create a patient panel that are all paid for in that way. If the subset of health plans using Patient-Centered Primary Care Payment were those providing insurance for higher-need patients, then even if they insured fewer than half of the patients, a primary care practice could continue delivering care to those patients and receive enough revenue though Patient-Centered Primary Care Payment to cover its costs.
To illustrate this, Figure 21 shows the hypothetical primary care practice described earlier, assuming that its patients have insurance from three different health plans, and that the patients insured by the different plans have different levels of need.
- As shown in the first column (“Current”), assuming that all of the insurance plans currently pay the same fees for office visits as Medicare does, the practice has to have 2,500 patients in order to break even, but it is impossible for the single physician in the practice to provide high-quality care to the patients without working more than 17 hours per day.
- Column 2 assumes that Plan A and Plan B begin using Patient-Centered Primary Care Payment and Plan C does not. Although Plans A & B only insure 40% of the practice’s current patients, those patients have more chronic conditions than the patients insured by Plan C, and so they represent a much higher share of the practice’s time and revenues. If the practice only continues to serve the patients insured by Plan A and Plan B (and no longer takes care of the patients with insurance from Plan C), it would have a total of 1,000 patients, the practice would have additional staff and sufficient time to provide high-quality care to those patients, the practice would receive Patient-Centered Primary Care Payment for all of the patients, and the practice would have sufficient revenue to cover its costs.
- Column 3 assumes the opposite – that Plan C begins using Patient-Centered Primary Care Payment and Plans A and B do not. If the practice only continues to serve the 1,500 patients insured by Plan C (and no longer takes care of the patients with insurance from Plans A and B), the amounts received under Patient-Centered Primary Care Payment would generate sufficient revenue to enable the practice to provide high-quality care to those patients.
- Ideally, all three health insurance plans would use Patient-Centered Primary Care Payment. Column 4 shows that in this case, the practice could retain all of its existing patients and provide high-quality care to them by hiring an additional primary care physician, and it would have adequate revenues to do so.
FIGURE 21
Impact of Non-Participating Payers
on a Hypothetical Primary Care Practice
| Current | Patient-Centered Payment from Payers A and B |
Patient-Centered Payment from Payer C |
Patient-Centered Payment from All Payers |
|
|---|---|---|---|---|
| Total Patients | 2,500 | 1,000 | 1,500 | 2,500 |
| % with Chronic Condition | 40% | |||
| Total Visits Per Year | 2.30 | |||
| Acute Visits Per Year | 1.25 | |||
| Payer A | ||||
| % of Original Patients | 100% | 0% | 100% | |
| Patients | 375 | 375 | 0 | 375 |
| % with Chronic Condition | 80% | 80% | 80% | |
| Acute Visits Per Year | 1.25 | 2.00 | 2.00 | |
| Payer B | ||||
| % of Original Patients | 100% | 0% | 100% | |
| Patients | 625 | 625 | 0 | 625 |
| % with Chronic Condition | 45% | 45% | 45% | |
| Acute Visits Per Year | 1.40 | 1.40 | 1.40 | |
| Payer C | ||||
| % of Original Patients | 0% | 100% | 100% | |
| Patients | 1,500 | 0 | 1,500 | 1,500 |
| % with Chronic Condition | 29% | 29% | 29% | |
| Acute Visits Per Year | 1.00 | 1.00 | 1.00 | |
| Patient Revenues | ||||
| FFS Visit Revenue | $462,547 | |||
| Wellness Care Revenue | $88,800 | $133,200 | $222,000 | |
| BH Care Revenue | $51,000 | $76,500 | $127,500 | |
| Acute Care Revenue | $229,125 | $211,500 | $440,625 | |
| Chronic Care Revenue | $213,435 | $156,978 | $370,413 | |
| Total Revenue | $462,547 | $582,360 | $578,178 | $1,160,538 |
| Practice Expenses | ||||
| Physician | $250,000 | $250,000 | $250,000 | $500,000 |
| Nurse/BH Care Manager | $80,000 | $80,000 | $160,000 | |
| Other Staff/Benefits | $140,400 | $156,400 | $156,400 | $312,800 |
| Other Practice Costs | $62,400 | $91,250 | $91,250 | $182,500 |
| Total Expenses | $452,400 | $577,650 | $577,650 | $1,155,300 |
| Profit/Loss | $10,147 | $4,710 | $528 | $5,238 |
| Number of Physicians | 1 | 1 | 1 | 2 |
| Physician Hours Per Day | ||||
| Preventive Care | 3.2 | 1.3 | 1.9 | 1.6 |
| Acute Care | 7.3 | 3.8 | 3.5 | 3.6 |
| Chronic Condition Care | 6.4 | 3.7 | 2.7 | 3.2 |
| Open Slots | 0.5 | 0.5 | 0.5 | 0.5 |
| Total Time | 17.4 | 9.3 | 8.6 | 8.9 |
A primary care practice would not be limited to its current patients when it tries to create a panel of patients supported by Patient-Centered Primary Care Payment. If a patient has an insurance plan that uses Patient-Centered Primary Care Payment, but the patient is currently receiving care from a primary care practice that is unwilling to change the way it delivers care, that patient could enroll in the practice that is providing patient-centered care.
If one of the current patients in a primary care practice wants to continue receiving care from the practice, but the patient’s insurance plan is unwilling to use Patient-Centered Primary Care Payment, the patient can do one of two things:
Change health insurance plans. If the patient has a choice of which health insurance plan to use, he or she can switch to a health insurance plan that does pay using Patient-Centered Primary Care Payment. Patients are accustomed to choosing health insurance plans based on whether their current or preferred physicians are “in-network” for that plan, so if their preferred primary care practice either stops contracting with the patient’s current health plan or indicates that it will only be accepting patients whose health insurance plan uses Patient-Centered Primary Care Payment, the patient can switch to a different health plan. For example, Medicare beneficiaries are annually asked to choose between receiving coverage under Original Medicare or one of many Medicare Advantage plans. Decisions to date have been based primarily on premiums charged, out-of-pocket costs, and extra benefits offered. However, one of the most important factors that the beneficiaries should be considering is whether they will be receiving high-quality primary care, so it will be important for them to begin asking how Original Medicare or a Medicare Advantage plan is paying their primary care physician and choosing the option that will enable them to receive the best care.
Pay out of pocket for primary care. If a patient cannot or does not want to change insurance plans, but has the ability to pay for primary care services directly, the patient could simply pay the Patient-Centered Primary Care Payment amounts to the primary care practice for the services they enroll for and receive. Some patients with high-deductible insurance plans may already be paying out-of-pocket for much of their primary care, so the change in spending for them could be small, while the improved quality of care would be significant. Direct Primary Care practices have demonstrated that there are many patients with insurance coverage for primary care who will pay completely out-of-pocket to receive high-quality primary care; the payments under Patient-Centered Primary Care Payment would be significantly less than the amounts typically charged by Direct Primary Care practices.79
If patients stop using health insurance plans that do not use Patient-Centered Primary Care Payment, that creates a financial incentive for those insurance plans to change the way they pay for primary care. As a result, fewer patients may need to switch health plans than might initially appear necessary. However, some patients will likely need to switch plans in order to signal that the way health plans support high-quality primary care is important to them.
If a health insurance plan is paying very high fees for office visits to a primary care practice, the practice could decide to temporarily continue providing care to patients insured by that plan, even if the plan is not willing to use Patient-Centered Primary Care Payment, since the financial loss from doing so would be less than for other plans. If a health plan is already paying high fees, the plan is already spending more on primary care than other payers, so switching to Patient-Centered Primary Care Payment would likely not increase the plan’s spending significantly. As a result, it should be easier to convince such a plan to implement Patient-Centered Primary Care Payment. However, if the plan does not do so, the practice will have higher administrative costs because of the different payment method, so it would not be desirable for a practice to do this for many patients or for a long period of time.
It may appear that paying adequately and appropriately for primary care using Patient-Centered Primary Care Payment would reduce access to primary care, since more physicians will be needed to provide primary care to current patients. However, the problems with the current payment system are already creating problems accessing primary care by discouraging doctors from becoming primary care physicians and causing existing physicians to leave. If primary care physicians are paid in a way that enables them to provide high-quality care to patients within a reasonable workday, with fewer administrative burdens, and at a good salary, fewer existing physicians will stop practicing, and more physicians will enter primary care, thereby improving access for patients.
Patient-Centered Payment Compared to Other Approaches
There is no perfect payment system for primary care or any other aspect of healthcare services. Every payment system has strengths and weaknesses, including the Patient-Centered Primary Care Payment system described in the previous section. The key questions are:
- Will Patient-Centered Primary Care Payment be better than other payment systems in enabling and assuring delivery of high-quality care to each patient?
- Will Patient-Centered Primary Care Payment do a better job than alternatives in providing adequate financial support for primary care practices?
Comparison to Current Fee-for-Service Systems
There are four specific problems with current fee-for-service payment systems that have prevented physician practices from delivering high quality primary care to patients: (1) the lack of any fees at all for some important services, (2) inadequate fees for other important services, (3) paying fees regardless of the appropriateness or quality of care delivered, and (4) financially penalizing practices that keep their patients healthy. In order to be better than current payment systems, an alternative approach needs to reduce or eliminate these problems.
Figure 22 shows that Patient-Centered Primary Care Payments would specifically address each of the problems in the current fee-for-service system.
FIGURE 22
Comparison of Fee-for-Service Payment and
Patient-Centered Primary Care Payment
|
Problems with Fee for Service Payment |
Solutions Under Patient-Centered Primary Care Payment |
|---|---|
| There are no fees for delivering proactive care and non-visit-based services. | The monthly payments for wellness care and chronic condition management allow delivery of proactive care. The fees for addressing acute problems allow services to be delivered in the most appropriate way for each patient, including both office visits and telehealth. |
| The fees for services are less than what it costs to deliver high-quality care. | The payment amounts for each service are explicitly designed to be adequate to cover the estimated costs a primary care practice would incur to deliver high-quality services to an appropriately sized patient panel |
| There is no assurance that a patient has received appropriate, high-quality services when a fee is paid. | The primary care practice is only paid for a month of care or an acute visit for an individual patient if the physician and practice staff have delivered appropriate, evidence-based care to that specific patient or documented reasons for deviations. |
| The primary care practice loses money if it succeeds in keeping its patients healthy. | The primary care practice receives the monthly wellness care and chronic condition management payments for a patient even if the patient is healthy and does not need any treatments during the month. |
Comparison to Population-Based Payment/Capitation
It is important to recognize that the problem with the current payment system is not the fact that physicians are paid fees for delivering services to patients; the problem is the decisions Medicare and health plans have made about which services will receive fees and how large those fees will be. A corollary of this is that an alternative payment system will not automatically be better simply because it does not pay fees for individual services.
The Problems with Population-Based Payments
In fact, as discussed in Section 3-C, capitation payments and population-based payments – which in their purest forms do not pay any fees for individual services at all – address some but not all of the problems in fee-for-service payment. Most population-based payments are designed to provide a primary care practice with the same amount of revenue as it received under fee-for-service payment, so they are still not adequate to support the cost of delivering high-quality primary care. More importantly, population-based payments provide even less assurance that patients will receive high-quality care than current fee-for-service systems, because a physician practice will still be paid even if a patient does not receive the services they need.
Patient-Centered Primary Care Payment solves the problems with fee-for-service while avoiding the problems with population-based payments. Figure 23 shows how Patient-Centered Primary Care Payment addresses each of the weaknesses and problems with population-based payments.
FIGURE 23
Comparison of Population-Based Payment and
Patient-Centered Primary Care Payment
|
Problems with Population-Based Payment (Risk-Adjusted Capitation) |
Payment Under Patient-Centered Primary Care Payment |
|---|---|
| The monthly payment amounts may not be adequate to cover the practice's costs. | The payment amounts for each service are explicitly designed to adequately cover the cost of delivering high-quality care to an appropriately sized patient panel. |
| The primary care practice receives a monthly payment for each patient, regardless of whether the patient received the services they need. | The primary care practice is only paid for a month of care or an acute visit for an individual patient if the physician and practice staff have delivered appropriate, evidence-based care to that specific patient or documented reasons for deviations. |
| The primary care practice is paid the same amount for a patient with a chronic condition regardless of whether the practice is providing the care for that chronic condition or the patient is receiving care from a specialist. | The primary care practice is paid more to provide care management for a patient with a chronic condition, but only if the patient has enrolled with the practice for that care and the practice actually provides it. |
| The primary care practice is paid the same amount for a patient who has been newly diagnosed with a chronic disease. (Commonly-used risk adjustment systems only consider diagnoses assigned during the previous year.) | The primary care practice receives a higher payment for management of a chronic disease as soon a patient is diagnosed with the condition and agrees to enroll for services. |
| The monthly payment to the primary care practice is the same even if a patient experiences many acute problems during the year. (Commonly-used risk adjustment systems do not adjust for acute conditions.) | The primary care practice is paid more each time a patient has a new acute problem, enabling the practice to spend adequate time on diagnosis and treatment of each acute problem. |
| The primary care practice is paid the same amount for a patient who faces non-medical barriers to receiving healthcare services and improving health, such as poverty, homelessness, illiteracy, lack of access to transportation or fresh food, etc. | The primary care practice is paid more for patients with characteristics that make their care significantly more complex. |
Why Population-Based Payments Don’t Support Patient-Centered Care
Some of the advantages of Patient-Centered Primary Care Payment compared to Population-Based Payments are easier to see by looking at how payments align with the cost of meeting the needs of individual patients. Population-Based Payments are even less patient-centered than fee-for-service payments because they are, by definition, focused on what is needed on average for a group of patients rather than what is needed by each individual patient. If the payments are the same for all patients in a primary care practice, or the same for all patients with the same diagnoses, the payments will be inherently be less than necessary for patients who have greater needs and higher than necessary for healthier patients who need less assistance.
For example, Figure 24 shows eight hypothetical patients who might be receiving primary care from the hypothetical practice described in Figure 8 of Section 4-D. Each of the patients requires a different set of services from the primary care practice to address their healthcare needs; some have a chronic condition and some do not; some have multiple acute problems during the year and some have none; one is diagnosed with cancer and receives most of their care during the year from an oncology practice rather than the primary care practice. Figure 24 shows an estimate of the cost the primary care practice incurs delivering services to each patient, based on the services the patients need from the practice, the estimated amount of time required to deliver the services, and the unit costs of the services as estimated in Section 4-D.
FIGURE 24
Relative Annual Cost of Primary Care Services
for Different Types of Patients
| Chronic Condition Managed by Practice |
Acute Problems During the Year |
Primary Care Services Needed | Wellness Care |
Acute Care |
Chronic Condition Care |
Total Annual Primary Care Cost |
|---|---|---|---|---|---|---|
| None | None | Wellness Care Only | $89 | $0 | $0 | $89 |
| None | One | Wellness Care + Acute Visit |
$89 | $141 | $0 | $230 |
| None | Three | Wellness Care + Multiple Acute Visits |
$89 | $423 | $0 | $512 |
| Non-Complex | None | Wellness Care + Chronic Condition Mgt |
$89 | $0 | $367 | $456 |
| Non-Complex | One | Wellness Care + Chronic Care + Acute Visit |
$89 | $141 | $367 | $597 |
| Non-Complex | Three | Wellness Care + Chronic Care + Multiple Acute Visits |
$89 | $423 | $367 | $879 |
| Complex | Two | Wellness Care + Complex Condition Mgt + Acute Visits |
$89 | $282 | $734 | $1,105 |
| None | Cancer | Wellness Care (+ Cancer Care from Oncologist) |
$89 | $0 | $0 | $89 |
Assuming the patients in the practice have the same overall characteristics as assumed in Figure 8 (i.e., 40% have a chronic condition and the patients visit the practice on average 1.25 times per year for acute needs), the practice would have to receive a capitation payment of $33.63 per month for every patient in order to cover its costs over the course of the year. As shown in Figure 25, this amount would be much higher than the cost of providing care for the healthiest patients and for patients receiving most of their care from a specialist, whereas it would be far less than the cost of providing primary care to the patients with the greatest needs.
FIGURE 25
Capitation Payment vs. Cost of Primary Care Services
for Different Types of Patients
| Chronic Condition |
Acute Problems |
Primary Care Services Needed | Primary Care Cost |
Capitation Payment |
Difference From Cost |
|
|---|---|---|---|---|---|---|
| None | None | Wellness Care Only | $89 | $412 | $323 | |
| None | One | Wellness Care + Acute Visit |
$230 | $412 | $182 | |
| None | Three | Wellness Care + Multiple Acute Visits |
$512 | $412 | ($100) | |
| Non-Complex | None | Wellness Care + Chronic Condition Mgt |
$456 | $412 | ($44) | |
| Non-Complex | One | Wellness Care + Chronic Care + Acute Visit |
$597 | $412 | ($185) | |
| Non-Complex | Three | Wellness Care + Chronic Care + Multiple Acute Visits |
$879 | $412 | ($467) | |
| Complex | Two | Wellness Care + Complex Condition Mgt + Acute Visits |
$1,105 | $412 | ($693) | |
| None | Cancer | Wellness Care (+ Cancer Care from Oncologist) |
$89 | $412 | $323 | |
In aggregate, the high and low payments could “average out” to an adequate total amount of revenue for the practice, but this would only happen if the characteristics of the patients in the practice are similar to those used in determining the capitation payment amount. If a primary care practice takes on more patients with chronic conditions, or if its patients develop chronic conditions as they age, then the practice will no longer be able to provide care for the same number of patients at the same cost, and the capitation payment will no longer generate sufficient revenues to cover the cost of caring for those patients.
Moreover, if every primary care practice receives the same capitation payment amount, rather than an amount customized to the types of patients in the practice, primary care practices that are providing care to higher-need patients will lose money and the practices providing care primarily to younger, healthier patients will be very profitable. This would encourage primary care practices to “cherry-pick” patients, and it could make it harder for higher-need patients to find a primary care practice willing and able to provide care for them.
Why Risk-Adjustment Fails to Solve the Problem
Population-based payment systems that “risk adjust” the capitation payments do not solve the problem. Typical risk adjustment systems, such as the Hierarchical Condition Category (HCC) risk adjustment system used in Medicare payment programs, are designed to predict total spending on all health services delivered to a group of patients in future years, not to predict the amount of time the primary care practice will need to spend caring for an individual patient in the current year. In particular, standard risk adjustment systems:
- assign a higher risk score to a patient who had a chronic condition during the previous year, but not to a patient newly diagnosed with the chronic condition in the current year, even though the largest investment of time by the primary care practice will likely be needed when a chronic condition is first diagnosed and initially treated;
- do not change a patient’s risk score because of acute problems the patient experiences during the year, no matter how many acute problems there are or how much time is required to accurately diagnose and treat those problems;
- do nothing to adjust for non-medical characteristics of patients that create barriers to receiving healthcare services and doing things that are necessary to maintain and improve their health, such as poverty, homelessness, illiteracy, lack of access to transportation and fresh food, etc.80
- determine relative risk scores based on differences in total healthcare spending on the patient, not based on differences in the amount of time a primary care practice would need to spend managing their care.
For example, in the Medicare HCC risk adjustment system:
- A 66-year-old male with no other health problems would be assigned a risk score of 0.308.
- If that same 66-year-old male had pneumonia or an injury during the year, the risk score would still be 0.308.
- A 66-year-old male with uncomplicated diabetes and no other health problems would be assigned a 34% higher risk score of 0.413 (0.308 + 0.105).
- A 66-year-old male with uncomplicated diabetes but who had limited income and lacked access to transportation would also be assigned a 34% higher risk score of 0.413, since there is no adjustment for income or access to transportation.
- A 66-year-old male who was diagnosed with cancer would still have a risk score of 0.308 if the cancer was diagnosed in the current year; however, if the cancer was diagnosed in the previous year, the risk score in the current year would be significantly higher (e.g., 0.615 if he had bladder cancer), even though it is likely the man would be receiving a significant portion of his care from an oncologist or urologist, rather than the primary care practice.
Figure 26 shows that even if the population-based payment amount for healthy patients was set to match the cost of preventive care and one acute visit during the year, and if the payments for patients with chronic conditions were adjusted in proportion to the HCC risk scores that might be assigned to these patients, the payment amounts for most of the individual patients would still differ significantly from the estimated costs of providing the services they need, thereby penalizing a practice with a larger number of patients who have chronic conditions and multiple acute problems.
FIGURE 26
Population-Based Payment vs. Cost of Primary Care Services
for Different Types of Patients
| Chronic Condition |
Acute Problems |
Primary Care Services Needed | Primary Care Cost |
Risk Score | Population- Based Payment |
Difference From Cost |
|---|---|---|---|---|---|---|
| None | None | Wellness Care Only | $89 | 0.56 | $231 | $142 |
| None | One | Wellness Care + Acute Visit |
$230 | 0.56 | $231 | $1 |
| None | Three | Wellness Care + Multiple Acute Visits |
$512 | 0.56 | $231 | ($281) |
| Non-Complex | None | Wellness Care + Chronic Condition Mgt |
$456 | 0.75 | $309 | ($147) |
| Non-Complex | One | Wellness Care + Chronic Care + Acute Visit |
$597 | 0.75 | $309 | ($288) |
| Non-Complex | Three | Wellness Care + Chronic Care + Multiple Acute Visits |
$879 | 0.75 | $309 | ($570) |
| Complex | Two | Wellness Care + Complex Condition Mgt + Acute Visits |
$1,105 | 0.75 | $309 | ($796) |
| None | Cancer | Wellness Care (+ Cancer Care from Oncologist) |
$89 | 1.12 | $461 | $372 |
Comparison to Pay-for-Performance Systems
Because neither fee-for-service payments nor capitation payments do anything directly to assure that patients are receiving high-quality care, many payers use some form of “pay-for-performance” system or add a “performance-based payment” component that increases or decreases payments based on the provider’s score on a group of quality measures. In addition, in order to encourage the delivery of appropriate care and discourage unnecessary services, payments may also be adjusted based on measures of service utilization or total spending. However, for the reasons described in Section 3-A, these performance-based payments are not designed in ways that will improve the quality of primary care or reduce overall spending on healthcare services.
The Problems With Pay-for-Performance
Figure 27 shows how the quality assurance mechanisms under Patient-Centered Primary Care Payment solve the problems with current performance-based payment systems and assure that each individual patient will receive both appropriate and high-quality care.
FIGURE 27
Comparison of Performance-Based Payment and
Patient-Centered Primary Care Payment
|
Problems with Performance-Based Payment |
Quality Assurance Under Patient-Centered Primary Care Payment |
|---|---|
| A primary care practice is deemed to be giving “good” quality care even if a significant fraction of the practice’s patients fails to receive evidence-based care or fails to achieve the outcome that is being measured, as long as the proportion of patients receiving poor quality care is smaller than the proportion in other practices. | Every patient is expected to receive evidence-based care appropriate to their needs, and there is no payment for a patient if that patient does not receive appropriate, high-quality care (unless the patient is unable or unwilling to accept the services). |
| There is no measure of quality for many types of patients and health problems, and no penalty for delivering poor quality care to those patients. | The primary care practice is only paid for care to a patient if the practice delivers services based on evidence-based guidelines that are applicable to the specific health problems of that individual patient. |
| The practice is not paid for any services needed to improve outcomes for patients that are not paid for under standard payments. | The payments to the primary care practice allow the flexibility to deliver the most appropriate and effective services to each patient, including services for which fees are not paid in current payment systems. |
| The performance standard required for the numerator of a quality measure may not be applicable to all patients included in the denominator, thereby penalizing the practice for avoiding the use of services that would be inappropriate for a patient. | The primary care practice is only expected to deliver services that evidence indicates would be safe and effective for the individual patient being treated. |
| Failure to achieve the performance standard required for the numerator of a quality measure may be due to the inability or unwillingness of the patient to receive evidence-based services, so the practice is penalized if its patients are unable or unwilling to use beneficial services. | The primary care practice is paid if the practice attempts to deliver the appropriate, evidence-based services needed to achieve good outcomes, and it is not penalized if the patient is unable or unwilling to accept the services. |
| Differences in performance on a quality measure between practices may be due to differences in the characteristics of their patients rather than differences in the quality of care delivered by the practices. | The primary care practice is expected to deliver evidence-based care to every patient, so any differences in outcomes will be due to factors other than differences in the quality of care delivered by the primary care practices. |
| The amount of the bonus for good performance may depend on how many other primary care practices performed poorly, which discourages collaboration among practices. | The primary care practice is paid if it delivers the appropriate, evidence-based care to the patient, regardless of what other practices do, and the practice is expected to participate in SCAMPs and to share information with other primary care practices in order to improve the quality of evidence about effective care. |
| Payments for primary care practices that perform well on quality measures are still less than the cost of the services needed to deliver high-quality care. | The amounts the primary care practice is paid for its services are designed to cover the cost of delivering high-quality services, so a practice that delivers high-quality care to all patients will not lose money. |
| If measures of total spending or spending on specialty services are used in addition to quality measures, the primary care practice could potentially receive higher payments if it does not order or deliver services that its patients need, and it could be penalized if the patients have health problems that require treatment using expensive medications or other services. | The primary care practice is accountable for delivering evidence-based care, and there is no financial reward or penalty based on the total amount spent on the patient's care. |
Why Performance-Based Payments Don’t Support Patient-Centered Care
The differences in the two approaches to quality assurance can be seen more clearly by examining how they would affect specific patients, such as patients with diabetes.
In performance-based payment programs, the most common approach to measuring the quality of diabetes care is calculating the percentage of diabetes patients whose glycated hemoglobin (HbA1c) level is higher than 9.0%.81 This measure is one of the “consensus core measures” for both primary care practices and Accountable Care Organizations (ACOs) that were selected by the Core Quality Measures Collaborative.82
The measure identifies the number of patients with poor diabetes control, not the number of patients with good control. Patients with diabetes have HbA1c levels higher than 6.5%, and one goal of diabetes care is to keep HbA1c levels as close to 6.5% as possible. However, some patients cannot achieve HbA1c levels as low as others without causing other health problems, so it is impossible to set a single standard for what is desirable and achievable for every patient. The 9.0% threshold is intended to identify an outcome that is undesirable for all patients, but even this approach has serious weaknesses:
- No distinction is made between patients whose HbA1c levels are only slightly lower than 9.0% and those whose levels are significantly lower, so a primary care practice that is achieving good outcomes for its patients can have the same score as a practice with only mediocre performance. Moreover, if patients had HbA1c levels below 8.0% or 7.0% and experienced an increase in their HbA1c levels, there would be no change in the measure as long as the HbA1c level remained below 9.0%.
- On the other hand, a primary care physician is not permitted to exclude patients from the calculation even if it is inappropriate or infeasible to reduce the HbA1c level below 9.0%, e.g., if the patient cannot afford the medications needed to achieve this level or refuses to take them. Patients are also included regardless of how long they have been under the care of the primary care practice, and regardless of how high their HbA1c level was when they first began receiving care from the practice. As a result, even if a primary care practice is delivering the most appropriate care to the patients and achieving the best results possible during the time the patient has been receiving care from the practice, the practice can appear worse on the quality measure than practices whose patients are better able to achieve good outcomes.
- In addition, if a diabetic patient in the primary care practice is receiving his or her diabetes care from an endocrinologist or other specialist rather than the primary care practice, the outcome for that patient is still used in measuring the quality of the primary care practice’s care.
As shown in Figure 28, national data indicate that on average, every year, 20-45% of patients with diabetes receive poor quality diabetes care as defined by the measure.83 The percentage has remained essentially unchanged for over a decade, despite the use of this measure in many payment incentive programs that were intended to encourage improvement. Because of the problems with the way the measure is defined, however, it is impossible to determine why performance is low.
FIGURE 28
Percentage of U.S. Patients
With Poor Diabetes Control
(>9.0% HbA1c)
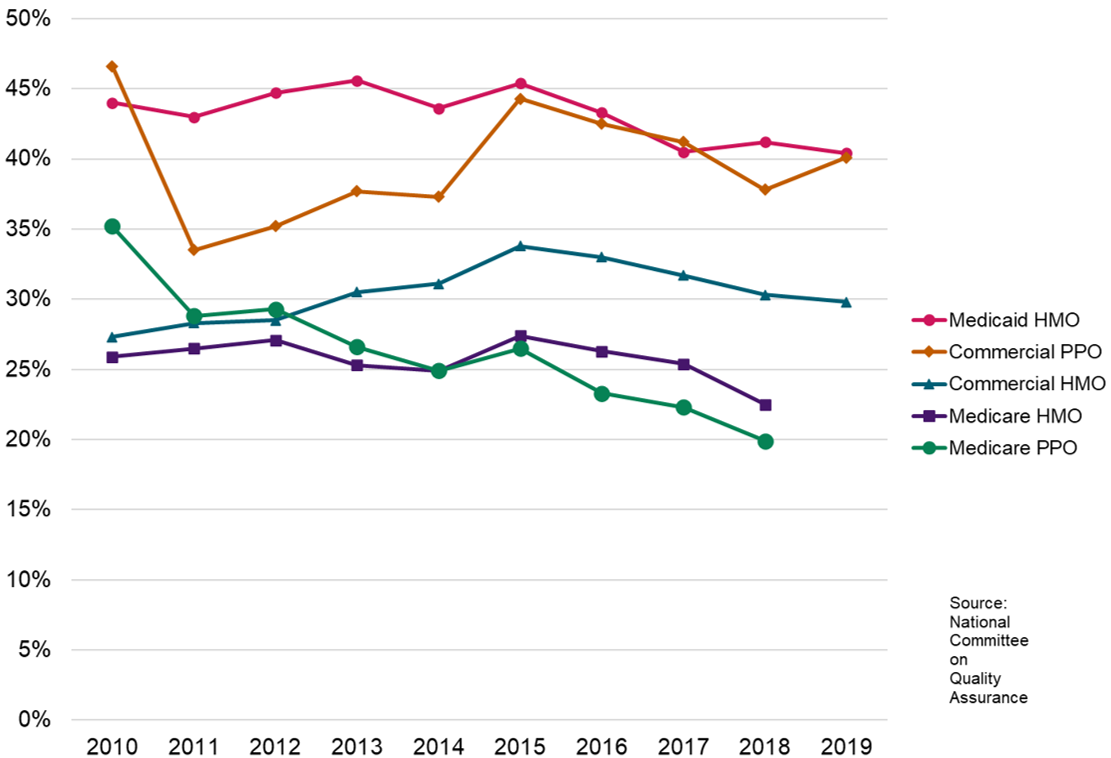
In contrast, in Patient-Centered Primary Care Payment, if the patient has enrolled with the primary care practice to receive diabetes care, the practice will only be paid for diabetes care if the practice has delivered or ordered all of the medications, treatments, and other services that evidence indicates will achieve the best outcomes for the patient (unless the patient is unable or willing to accept those services). Although maintaining a low HbA1c level will generally be one of the goals of diabetes care, it may not be the most important one depending on the patient’s specific needs, so the fact that a patient has an HbA1c level higher than 9.0% does not necessarily mean that the patient is receiving poor quality care.84
Figure 29 shows how Patient-Centered Primary Care Payment avoids each of the problems associated with this approach to quality measurement and ensures that each patient is receiving the most appropriate care.
FIGURE 29
Assessment of Quality Under Performance-Based Payment and
Patient-Centered Primary Care Payment
| Patient Scenario | How the Quality of Care Would Be Rated Under: | |
|---|---|---|
| Performance-Based Payment |
Patient-Centered Primary Care Payment |
|
| A patient with poorly controlled diabetes joins the primary care practice; the practice delivers evidence-based care to the patient, and their HbA1c level improves from 13% to 10% in the first year | Poor quality care | Good quality care |
| A patient with well controlled diabetes joins the primary care practice; the practice fails to deliver evidence-based care to the patient, and their HbA1c level worsens from 7.0% to 8.0% in the first year. | Good quality care | Poor quality care |
| A patient with poorly controlled diabetes cannot afford the medications needed to reduce their HbA1c levels, but the primary care practice is able to help the patient learn how to manage their diabetes without medication in a way that prevents them from getting worse. | Poor quality care | Good quality care |
| A patient with poorly controlled diabetes refuses to take prescribed medications or to take other actions recommended by the primary care practice to help them manage their diabetes despite repeated efforts by the practice to encourage and assist them to do so. | Poor quality care | Good quality care |
| A patient with diabetes is not prescribed the proper medications nor given any other assistance in managing their condition by the primary care practice, but the patient is able to keep their HbA1c level at 8% by following advice from friends. | Good quality care | Poor quality care |
Why Primary Care Practices Cannot Be Accountable for “Total Cost of Care”
Concerns about the high and growing cost of healthcare have caused many payers to add “Total Cost of Care” to the list of performance measures for which primary care practices are rewarded or penalized. The primary care practice may be penalized if the total amount of healthcare spending on its patients, including spending on services delivered by hospitals and specialists, is higher than the average spending for patients in other practices, and/or the practice may be penalized if the increase in total spending on its patients is higher than the increase in spending for patients in other practices.
The vast majority of the total amount a health insurance plan spends on healthcare for its members goes to services delivered by providers other than the primary care practice. National estimates indicate that on average, less than 10% of total healthcare spending goes to primary care practices; the rest pays for medications, laboratory tests, imaging studies, inpatient and outpatient hospital procedures, etc.
A primary care physician can certainly influence which services a patient receives from other providers based on what types of tests, medications, and procedures the physician orders, but a primary care physician cannot control what services the patients will receive or how much those services will cost:85
- Patients who have serious health problems such as cancer will need to be treated for those health problems. The cost of treatment for a single patient can be extremely high, so if a primary care practice happens to be providing primary care to one of those patients, the “total cost of care” for the primary care practice can increase significantly because of the misfortune of one patient.
- For example, the rate of new lung cancer diagnoses each year is about 300 per 100,000 Medicare beneficiaries. If a primary care practice has 1,250 total patients and 250 (20%) of those patients are Medicare beneficiaries, the practice could expect that every other year, one of its Medicare patients will be diagnosed with lung cancer. Treatment for lung cancer can cost as much as $100,000, depending on the type of lung cancer, whereas the average amount Medicare spends each year on the average Medicare beneficiary is about $10,000. Consequently, the total cost of care for the Medicare beneficiaries in the practice could increase or decrease by 4% each year solely based on whether one patient was diagnosed with lung cancer.86
- Under the most common fee-for-service payment systems and patient benefit designs, patients have the freedom to see multiple physicians and other providers, even for the same health problems. Each of the physicians and other healthcare providers involved in the patient’s care makes their own decisions about how to deliver services, and those individual decisions can independently increase or decrease the number or cost of services the patient receives, with no involvement or influence by the primary care physician.
- Outside of Medicare, the amounts health plans pay for laboratory tests, imaging studies, and outpatient procedures vary dramatically depending on where a patient receives the test or procedure. Although those differences in payments have a significant impact on total spending for patients, most primary care practices have no information on what the differences in costs are between different facilities, so it is inappropriate to hold them accountable for the differences.
Advocates for total cost of care measures argue that they give the primary care physician an “incentive” to take actions to reduce spending by other physicians and providers, but if the physician cannot reasonably expect to influence that other spending, using the total cost of care measure will likely have little impact on spending. Since their patients may have to pay all or part of the difference in cost, particularly those patients who are on high-deductible health plans, primary care practices will want to refer them to the facility that will deliver a high-quality service at the lowest cost, which will help control the total cost of care for their patients. To do that, however, the primary care practice needs to know what the differences in costs are and how much of the cost their patients would have to pay, and most primary care practices do not have access to that information.
Of even greater concern, however, is that use of total cost of care measures could discourage primary care practices from accepting patients who have serious health problems or who have characteristics (e.g., homelessness, low income, etc.) that place them at higher risk of developing such problems. The methodologies that are typically used to “risk adjust” total cost of care measures do not accurately predict total spending even for very large populations of patients, much less the small number of patients managed by a primary care practice. As discussed earlier in conjunction with population-based payments, risk adjustment systems do not even take into consideration acute conditions, new chronic diseases, or social determinants of health. (For example, Medicare’s Hierarchical Condition Category system would make no adjustment in expected spending during the year if a patient had a new diagnosis of lung cancer, even though that would clearly be expected to increase total Medicare spending significantly.)
Comparison to Medical Home (Hybrid) Payment Systems
The Structure of Medical Home Payment Models
A number of “medical home” payment programs have been created by Medicare and other payers in an effort to improve the quality of care and financial viability of primary care practices. In addition to paying fees for traditional office visits, most of these programs have included some type of monthly per-patient payment that is supposed to enable the primary care practice to deliver services for which there is no fee under standard fee-for-service systems or where the current fees are inadequate.
Although these “hybrid” payment models may appear similar to the Patient-Centered Primary Care Payment system described in Section 4 because both use a combination of fees and monthly payments per patient, the two approaches are very different both in structure and effect.
- For example, most medical home payment models continue to pay a fee for every office visit, including visits for exacerbations of a chronic disease, visits to address preventive care needs, and repeat visits for acute problems that were not correctly addressed the first time.
- Moreover, the monthly payments are paid only for patients who are “attributed” to the practice based on the number of office visits they make. As a result, if the primary care practice helps patients avoid chronic disease exacerbations, if it can ensure patients receive appropriate preventive care through telephone or email contacts with nurses or medical assistants rather than asking a patient to come to the primary care office, or if it can address an acute problem effectively in a single visit, the primary care practice is penalized financially by lower office visit revenues and fewer attributed patients.
In contrast, the Patient-Centered Primary Care Payment system only pays a fee for office visits to address new acute problems, and the monthly payments are received for any patient who enrolls for care, regardless of how many office visits they make, so there is no such penalty.
The medical home payment models also typically include some type of “performance-based payment” tied to quality measures. However, this has the same flaws described earlier with pay-for-performance systems. Although the monthly payments may enable the primary care practice to deliver higher quality care, the performance-based payments do little or nothing to assure that every patient receives high-quality care.
Figure 30 shows a side-by-side comparison of the significant differences in the structure of the Patient-Centered Primary Care Payment system and most current medical home payment models.
FIGURE 30
Comparison of Medical Home (Hybrid) Payment Systems
and Patient-Centered Primary Care Payment
| Type of Service | Component | Medical Home (Hybrid) Payment Systems |
Patient-Centered Primary Care Payment |
|---|---|---|---|
| Wellness Care | Payment Method | The PCP receives a small monthly payment for each attributed patient. In addition, the PCP receives a fee for each office visit with the physician for advice on preventive care. | The PCP receives a small monthly payment for each enrolled patient; the payment is the same regardless of whether the practice advises the patient during an office visit with a physician or other means that are more convenient and effective for the patient. |
| Quality Assurance | The PCP is paid for each patient and visit regardless of whether the patient received all evidence-based wellness and preventive care; the amount of the payment is only reduced if a high percentage of other patients have failed to receive specific screening exams. | The PCP does not receive the monthly payment for a patient if that patient did not receive all evidence-based wellness and preventive care services, unless the patient was unable/unwilling to do so. | |
| Acute Care | Payment Method | The PCP receives a fee for each in-person office visit with the physician for an acute problem; there is no fee if the problem is handled by phone or email. | The PCP receives a fee to address each new acute problem; the same fee is paid if the acute problem can be addressed through an office visit with the physician, through a telehealth contact with the physician, or by a member of the staff other than a physician. |
| Quality Assurance | The PCP is paid for an office visit regardless of whether the patient received appropriate services to diagnose and treat the problem; the PCP may be paid for multiple visits to deliver services for the same problem. | The PCP does not receive the fee if the patient did not receive evidence-based diagnosis and treatment for the acute problem (unless the patient was unable/unwilling to do so). | |
| Chronic Condition Care | Payment Method | The PCP receives a monthly payment for each attributed patient who was diagnosed with a chronic disease in the previous year; the payment may be higher if the patient has multiple chronic conditions or more severe conditions, regardless of whether the conditions are being treated by the PCP or a specialist. In addition, the PCP receives a fee for each office visit with the physician for treatment or management of a chronic condition. | The PCP receives a monthly payment for each enrolled patient who has a chronic disease, including patients who are newly diagnosed in the current year; the payment is higher for a patient with a complex condition, but the payment does not change based on whether services are delivered through office visits or other approaches. |
| Quality Assurance | The PCP is paid for each patient and visit regardless of whether the patient received all appropriate care for the chronic condition; the amount of the payment may be reduced if a high percentage of other patients with the chronic condition did not receive specific services or achieve specific outcomes. | The PCP does not receive the payment for a patient during a month if the patient has not received evidence-based services for their specific condition(s) (unless the patient is unable/unwilling to use those services). |
(In)Adequacy of Medical Home Payments
Even if the method of paying for services is desirable, if the amounts of payment are not adequate, the payment system will not enable patients to receive high-quality primary care. In contrast to Patient-Centered Primary Care Payment, the payments in most medical home payment systems have not been explicitly designed to cover the costs of high-quality primary care. Moreover, it has been difficult to determine whether the payments in these systems are adequate because of the ways in which the payments are structured.
Supplemental Payments in Addition to Standard Fees
In some medical home payment systems, the primary care practice receives payments that are explicitly intended to provide more revenue than the practice would have received under standard fee-for-service payments. In general, however, little or no effort has been made to ensure the amounts would be adequate to cover the costs of delivering high-quality primary care. Moreover, in most cases, the primary care practice is required to take on additional administrative tasks, hire specific kinds of staff, etc. as a condition of receiving the new payments, and these requirements increase the cost of operating the practice. If the additional payments are less than the additional costs, the primary care practice can end up worse off financially.
For example, in the Comprehensive Primary Care Plus (CPC+) payment program developed by the Center for Medicare and Medicaid Innovation (CMMI), primary care practices receive a monthly Care Management Fee (CMF) for each patient who is “attributed” to the practice, while continuing to receive standard fees for all office visits with the patients.87
- The amount of the CMF payment for an individual patient is based on the HCC risk score assigned to that patient by Medicare.
- The payments are also higher if the practice is participating in “Track 2” rather than “Track 1” of the program. On average, the payments are $15 per month for practices in Track 1 and $28 per month for practices in Track 2.
- CMMI has not provided any information justifying the differences in these amounts or showing that the amounts are individually or collectively adequate to cover the costs of the additional services the practices are expected to deliver.
Moreover, in CPC+, the payments described above are only for the subset of a practice’s patients who are Original Medicare beneficiaries; the evaluation of the program has found that other health plans are either not providing any additional payments at all or are providing much smaller payments for the patients they insure than Medicare is paying for its beneficiaries.88 The primary care practices participating in CPC+ have told evaluators that the payments they are receiving overall are not adequate to support the services they are being asked to deliver.
Population-Based Payments with Reduced Fees
In some medical home payment systems, the primary care practice receives new payments that are not intended to provide any additional revenue to the practice, but merely to give the practice greater “flexibility” in the way it delivers services than under standard fee-for-service systems, e.g., by not tying the practice’s revenue as closely to how many face-to-face office visits it delivers. Although this flexibility can be very helpful in enabling the practice to deliver care in a more patient-centered way, it may not reduce the costs of operating the practice; for example, a physician will generally need to spend as much or more time during a telehealth visit with a patient than during an office visit. Moreover, if the payments are based on the number of patients who had been receiving care at the practice under the fee-for-service payment system, then if the practice reduces the number of patients it is caring for so that it can spend more time with each patient, the practice will lose money.
For example, in Track 2 of the CMMI Comprehensive Primary Care Plus program, in addition to the supplemental Care Management Fees described earlier:
- primary care practices can receive a quarterly Comprehensive Primary Care Payment (CPCP) for each patient if the practice agrees to accept lower fees for office visits.
- practices can choose to receive either 60% of the standard office visit fees or 35% of the standard fees. The amount of the CPCP is then set so that it is approximately equal to 110% of the revenue the practice would be expected to lose through the reduced fees for visits.89 This means that the practice would only receive 4-6% more revenue through the combination of CPCP payments and reduced office visit fees than it would have received through standard office visit fees.90 Moreover, the primary care practice will still experience a reduction in revenue if patients make fewer visits to the practice, and since the CPCP was based on the number of patients the practice was seeing under the current payment system, if the practice reduces the number of patients it cares for, it will also receive less revenue.
In the CMMI Primary Care First program, which is the successor to the Comprehensive Primary Care Plus program, the primary care practice will not receive any Care Management Fees that are explicitly designed to provide more revenue.91
- The practice will be paid a $40.82 “Flat Visit Fee” for each office visit, which is less than half the average amount it would typically receive for office visits.
Most of the practice’s revenue will come from a new monthly “Professional Population-Based Payment” (PBP). - The amount of the PBP for a patient will depend on the average HCC risk score for all patients, not the risk score for the individual patient. If the patients in the practice have an average risk profile, as is likely for most primary care practices, the payment will be $28 per patient per month for every patient.
- The PBP amount will be reduced through a “leakage adjustment” if the patients in the primary care practice receive services from other primary care providers; the reduction in the PBP will be equal to the percentage of the patient’s total primary care visits made to other providers, e.g., if a patient makes 10% of their primary care visits during the year to a different primary care practice, the PBP will be reduced by 10%.
- CMMI has not provided any justification for how the PBP amounts were chosen, other than to indicate that, in combination with the Flat Visit Fees, participating primary care practices should expect to receive as much or more revenue as they would have received from traditional office visit fees.
Performance-Based Payments
The third approach to medical home payment systems has been to provide an increase in payment for the primary care practice if it achieves a specific performance threshold on measures of quality, the utilization of specific types of healthcare services by its patients (e.g., Emergency Department visits or hospital admissions), and/or the total amount of healthcare spending on all services the primary care practice’s patients receive from all providers. The amount of additional revenue a primary care practice will receive depends both on the sizes of the potential performance-based payments and the likelihood of achieving the levels of performance needed to receive them.
For example, in the CMMI Comprehensive Primary Care Plus Program, primary care practices can receive a “Performance-Based Incentive Payment” of up to $2.50 per month in Track 1 and up to $4.00 per month in Track 2, based on the practice’s performance relative to other primary care practices on a series of quality and service utilization measures. The maximum amounts represent only about 5-6% of the total revenues the practice could receive from all of the payments in the program, and most participating practices do not receive the maximum amounts.
In the Primary Care First program, the performance-based payment component is very large. The payments the practice receives from the Professional Population-Based Payments (PBP) and Flat Visit Fees can be increased by as much as 50%, or reduced by as much as 10%, based on the practice’s performance on quality and utilization measures. The primary determinant of this Performance-Based Adjustment is the rate at which the patients in the practice are hospitalized and how low that rate is compared to the patients in other practices. Because of the way the thresholds are defined, only a small percentage of practices could receive the maximum 50% increase, and for many, there may be little or no change in payment.92
Assessment of Current Medical Home Payment Programs
Figure 31 shows how much revenue the hypothetical primary care practice described in Section 4 might receive under the Medicare payment models described above and whether the revenue would be adequate to cover the cost of operating the practice. Since Medicare’s payment amounts are only designed for Medicare beneficiaries, it is necessary to assume that the practice is only providing care for Original Medicare beneficiaries in order to determine whether the payments are adequate to support high-quality primary care.
FIGURE 31
Revenues Under CMMI Demonstrations vs. Patient-Centered Primary Care Payment
| Standard FFS |
CPC+ Track 1 |
CPC+ Track 2 |
Primary Care First |
Patient- Centered Payment |
|
|---|---|---|---|---|---|
| Payments for Services | |||||
| Reduction in Fees | 40% | ||||
| Avg Payment Per Office Visit | $80 | $80 | $48 | $41 | |
| CPCP/PBP | $13.13 | $28.00 | |||
| Leakage Adjustment | $0.00 | -5% | |||
| Care Management Fee | $15.00 | $28.00 | |||
| Performance Incentive Payment | $2.50 | $4.00 | 20% | ||
| Wellness Care Per Month | $7.40 | ||||
| Acute Visit Payment | $141 | ||||
| Chronic Care Per Month | $30.60 | ||||
| Patient Service Revenues | |||||
| Office Visit Revenue | $277,528 | $277,528 | $166,517 | $142,360 | |
| CPCP/PBP Revenue | $0 | $0 | $122,112 | $260,400 | |
| Leakage Adjustment | $0 | ($13,020) | |||
| Care Mgt Fee Revenue | $0 | $139,500 | $260,400 | $0 | |
| Performance Revenue | $0 | $23,250 | $37,200 | $77,948 | |
| Wellness Care Revenue | $68,820 | ||||
| Acute Care Revenue | $218,550 | ||||
| Chronic Care Revenue | $227,664 | ||||
| Total Revenue | $277,528 | $440,278 | $586,229 | $467,688 | $515,034 |
| Total Practice Expenses | $504,400 | $504,400 | $504,400 | $504,400 | $504,400 |
| Profit/Loss | ($226,872) | ($64,122) | $81,829 | ($36,712) | $10,634 |
| Assumptions | |||||
| Total patients: | 775 | ||||
| % with chronic condition: | 80% | ||||
| Average total visits per year: | 4.5 | ||||
| Average acute visits per year: | 2.0 | ||||
Since Medicare beneficiaries are much more likely to have chronic conditions and have far more primary care visits than the general population, the calculations in Figure 31 assume that 80% of the patients in the practice have a chronic condition, that they would make about 4.5 visits per year to the practice under the current payment system, and that 2 visits per year are primarily for new acute problems. Since the Care Management Fees in the Medicare models differ based on the risk scores assigned to the patients, the calculations assume that the distribution of risk scores for the patients in the practice is similar to the distribution for all Medicare beneficiaries, i.e., the practice’s patients are “average” in terms of their risk scores.
Based on the estimated times required to deliver services discussed in Section 4, the hypothetical practice could only provide high-quality care to about 775 Medicare patients with these characteristics, rather than 1,250 patients of all ages as was assumed in the analyses in Section 4. The calculations in Figure 31 also assume that all of these patients would be formally assigned to the practice under CMS attribution rules (this means that the patients make at least one visit to the primary care practice and that they receive more of their primary care services from this practice than any other practice), so that the practice would receive monthly payments for every one of the patients.
Figure 31 shows that if the hypothetical practice was participating in Track 1 of CPC+ and if it received the maximum possible performance incentive payment, the practice would receive significantly more revenues than under standard fee-for-service payment, but the revenues would still be 12% less than the cost the practice would incur to deliver high-quality care. This assumes that the patients would continue to make office visits to the practice at the same rate as they did under fee-for-service payment. If the practice is able to address patients’ preventive care and chronic condition management needs without as many office visits, it would receive even less revenue because it is still paid for each office visit and most of its revenue would still be coming from office visit fees.
If the primary care practice was participating in Track 2 of CPC+, it could receive about 16% more revenue than needed to cover its costs. The difference in revenues between Track 1 and Track 2 is almost entirely due to the significantly higher Care Management Fees paid in Track 2. Since the practice is still being paid for all office visits, a reduction in the number of office visits would cause its revenues to decrease, but the impact would be lower than under Track 1 because the fees for office visits would be lower and a much smaller percentage of the total revenues come from office visit fees.
If the primary care practice was participating in Primary Care First, it would receive more revenue than it would receive under the current fee-for-service system, and more than under Track 1 of CPC+, but less than under Track 2 of CPC+ and less revenue than needed to cover its costs. The exact amount of revenue it receives will depend heavily on the exact amount of the Performance-Based Adjustment; the simulation in Figure 31 assumes a 20% upward adjustment, which is midway between the maximum upward adjustment of 50% and the maximum penalty of -10%. Although some practices could receive higher adjustments that would generate enough revenues to cover the cost of high-quality care, others would receive lower adjustments and experience greater losses. The amount of payment would also vary from year to year, potentially by large amounts, because of the way the Performance-Based Adjustment is determined.93
Since Patient-Centered Primary Care Payment is explicitly designed to cover the costs of delivering high-quality primary care, Figure 31 shows that the hypothetical practice would receive sufficient revenue to cover its costs. The proportions of the total revenue that come from each of the three different payment components (wellness care, acute care, and chronic care) are different than in the examples in Section 4 because the patients are all assumed to be Medicare patients who are more likely to have a chronic condition and more likely to have acute problems, but the total revenues still match the cost of operating the practice.
Comparison to ACOs and Global Payments
Because of the problems with traditional fee-for-service payments and because Medicare’s primary care payment demonstration projects have only been available to primary care practices located in specific states and regions, the only alternative that has been available to many primary care practices has been joining or forming an Accountable Care Organization (ACO).
An ACO is an organizational structure, not a payment system. As they were originally conceived, ACOs were expected to involve all of the physicians, including both primary care physicians and specialists, who were providing all or most of the services for a group of patients. By forming an ACO, it was believed that the physicians would have greater ability to coordinate their services and deliver patient care more efficiently and effectively. This, in turn, would enable the ACO physicians to collectively take accountability for the overall quality of care for the group of patients and reduce the total amount of money spent on that care.
Although it is very desirable for patients to receive more coordinated care, it does little good to coordinate services if the services themselves are not being delivered appropriately because of barriers in the payment system. Consequently, forming an ACO will have only limited benefit for patients if it is not accompanied by a better approach to paying the physicians for their services. Two basic approaches have been used (or proposed) for paying ACOs: (1) shared savings, and (2) global payments.
Shared Savings Payments
As part of the Affordable Care Act, Congress created a new program – the Medicare Shared Savings Program (MSSP) – allowing physicians who formed an ACO to be paid differently under Medicare. Although the law gave CMS the authority to create multiple approaches to paying ACOs, the only payment system that Congress required CMS to use was “shared savings” and that essentially has been the only approach CMS has used in the program.
Under the shared savings payment model, there is no change at all in the way that a primary care physician (or any other provider) is paid for delivering an individual service. Primary care physicians continue to be paid standard Medicare payment amounts for the services that Medicare pays for, and they are still paid nothing for the services that Medicare does not pay for. If CMS determines that the total spending on the Medicare beneficiaries that received primary care services from the physicians in the ACO is lower than CMS projects spending would have been in the absence of the ACO, CMS provides a bonus payment to the ACO based on a fraction of the estimated savings, i.e., the ACO receives a share of Medicare’s savings. However, it is impossible for the ACO or the physicians participating in it to know whether or not they will receive such a bonus payment or how large it will be until after services are delivered and after CMS calculates the spending and savings using a very complex formula.94
As a result, the Medicare Shared Savings Program is a form of pay-for-performance payment, and as such, it has the same types of problems described earlier regarding other types of pay-for-performance programs. The biggest difference from other pay-for-performance programs is that MSSP only provides a bonus payment if spending is reduced, not if the quality of care is improved with no change in spending. Poor performance on quality measures can reduce a bonus payment if savings has been achieved, but no matter how good the quality of care is, the bonus will never be higher than a predetermined percentage of the savings CMS calculates that Medicare has received.
Some primary care practices have been able to receive large bonus payments by participating in an ACO, but many ACOs have not qualified for any shared savings payments. Even ACOs that have received bonus payments do not receive such payments every year. Moreover, the bonus payments, if they are awarded, come long after services are delivered, since CMS has to first calculate the actual spending during the year in order to determine if savings have occurred.
Consequently, if a primary care practice that is part of an ACO hires a nurse or behavioral health specialist in order to deliver better care to its patients, it will incur the additional costs for doing so but additional revenue, if any, would come many months later. If the primary care practice reduces the number of office visits with patients and instead delivers care in more proactive ways, it will lose visit-based revenues immediately, but it would not receive a shared savings bonus until many months later, and there would be no assurance that the practice would receive any bonus at all, much less an amount that is greater than the revenue it had already lost.
Since the shared savings payment approach has failed to produce significant savings for Medicare, CMS is now requiring that all ACOs will have to accept “downside risk” if they want to receive shared savings bonuses, i.e., the ACO will have to pay a penalty if CMS calculates that total spending on the ACO patients has increased more than CMS believes it should have. This is even more problematic for small primary care practices, since they cannot control the services hospitals deliver, the price of drugs, and other factors that have a major effect on total spending, and they do not even receive enough revenue to cover the costs of delivering high-quality primary care, much less enough to pay penalties if spending on hospitals and drugs increases. As discussed earlier in conjunction with performance-based payments using total cost of care measures, it is both inappropriate and problematic to penalize primary care practices for changes in spending they cannot control.
There is no greater assurance that patients will receive high-quality care under the ACO program than under standard fee-for-service or pay-for-performance programs. In fact, there is even less assurance of quality care, because the physicians in the ACO could be penalized if the services they deliver or order for their patients would result in higher spending even if those services are necessary and appropriate, and the physicians could actually receive a bonus payment if they fail to deliver or order expensive services even if their patients need them.
Figure 32 compares how primary care practices would be paid under a shared savings payment model and under Patient-Centered Primary Care Payment.
FIGURE 32
Comparison of Shared Savings Payment and
Patient-Centered Primary Care Payment
|
Payments for Primary Care Services Under Shared Savings Payment |
Payments for Primary Care Services in Patient-Centered Primary Care Payment |
|---|---|
| The primary care practice receives standard fee-for-service payments for all services; there are no new fees for any services that are not currently paid for. | The primary care practice receives monthly payments for wellness care and chronic condition management, and higher payments for diagnosis and treatment of new acute problems. |
| The primary care practice can receive a shared saving bonus if it finds a way to keep patients healthier and reduce total spending, but the bonus payment will come long after the services are delivered. The bonus payment may or may not be large enough to cover any costs the primary care practice incurred for hiring new staff or any fee-for-service revenues it lost by delivering services differently. | The payments the practice receives are set at levels that are expected to be adequate to cover the costs of delivering those services. |
| The primary care practice can receive a shared savings bonus if it reduces spending by failing to deliver evidence-based services. | The practice is not paid unless it delivers or orders all appropriate, evidence-based services. |
| If the ACO is subject to downside risk, the primary care practice could be penalized financially if following evidence-based guidelines causing spending on the patients to increase. | The practice is paid adequately for delivering and ordering all appropriate, evidence-based services, even if that causes total spending on the patients to increase. |
Global Payments
A number of large physician practices, independent practice associations, and health systems have withdrawn from the Medicare Shared Savings Program or have refused to participate at all because of the problematic structure of the program and the fact that it makes no actual changes in the way physicians and other healthcare providers are paid for services. Some have called for Medicare to pay ACOs using a “global payment” instead. Many of these organizations already have capitation contracts with Medicare Advantage plans and commercial HMO plans that pay them in similar ways.
In response, CMS has created a new demonstration program called “Direct Contracting” in which entities called “Direct Contracting Entities (DCEs)” can take financial risk for the total Medicare spending on a group of assigned beneficiaries and receive capitation payments instead of fees for some or all of the services they provide.95
Whether one calls this “global payment,” “global capitation,” or “direct contracting,” and whether one calls the entity receiving the payment a DCE, ACO, or something else, the basic concept is the same:
- a group of healthcare providers (the DCE/ACO) receives a monthly payment for each Medicare beneficiary who is assigned to the group.
- the payment is determined by taking the average monthly amount that is being spent on all of the services the patients are currently receiving, and then reducing that amount by an arbitrary “discount” designed to reduce total spending for Medicare;
- the providers in the DCE/ACO no longer receive separate fees for the individual services they deliver to the assigned beneficiaries. They receive the same monthly amount of payment regardless of how many services or what kinds of services they deliver;
- the monthly payment amount is risk-adjusted based on changes in the patients’ chronic conditions, but the adjustments occur the year after a patient receives a new diagnosis, and there is no adjustment for acute illnesses;
- if a provider who is not a member of the DCE/ACO delivers a service to one of the beneficiaries who is assigned to the DCE/ACO, that provider is paid the standard Medicare fee for that service by CMS, and the monthly payments to the DCE/ACO are reduced by the amount of that fee. As a result, the total amount that Medicare spends on the assigned beneficiaries is equal to the monthly payments to the DCE/ACO to which those beneficiaries are assigned.
If a group of primary care practices were to accept such a global payment system, it would have the same advantages and disadvantages described earlier for population-based primary care payments as well as some of the problems associated with the shared savings approach:
- Monthly global payments would give the primary care practices far more flexibility in delivering services than either standard fee-for-service payment systems or the Shared Savings Program, since the monthly payments are not tied to how many or what types of services are delivered. For example, a primary care practice could use the payments to hire a nurse or deliver services through telehealth rather than office visits.
- However, the amount of payment for primary care services will probably be no higher than it is today, and likely less. Since the total monthly payments will be lower than the current level of spending due to the discount, and since hospitals and specialists that are not part of the DCE/ACO will continue to be paid at standard rates and the payments for their services will be deducted from the monthly payment, the amount remaining for the primary care practices will likely be less than what they currently receive.
- If the primary care practices in the DCE/ACO spend more on additional staff and information systems and are able to reduce overall spending as a result, the DCE/ACO will be able to retain the savings, but that may or may not be enough to pay for the amount the primary care practices spent to improve care.
- If spending on hospitals, specialists, or drugs outside of the DCE/ACO increase, the amount remaining for the primary care practices in the DCE/ACO could decrease significantly and be insufficient to cover even the current costs of the primary care practices’ services.
- There is no greater assurance that patients will receive high-quality care under the global payment system than under standard fee-for-service or pay-for-performance programs. In fact, there is even less assurance of quality care than there is today, because the physicians in the DCE/ACO could be penalized if the services they deliver or order for their patients would result in higher spending, even if those services are necessary and appropriate, and the physicians could receive a bonus payment if they fail to deliver or order expensive services even if their patients need them.
The financial risk for the providers in the DCE/ACO is much greater than under the Medicare Shared Savings Program. This risk may be manageable for a large physician organization or health system that orders and delivers most of the services that the assigned beneficiary receives, but it is not manageable for primary care practices that only order or deliver a small fraction of those services and that do not have significant financial reserves.
For example, Figure 33 shows a hypothetical group of Medicare beneficiaries with average total annual spending of $10,000 per beneficiary. The primary care practices for these beneficiaries receive an average of $500 in fee-for-service payments during the year, representing 5% of total spending.
- If the practices agree to accept a global payment for these patients that is based on current spending minus a 3% discount, and if there is no change in spending on specialists and hospitals, the amount of revenue remaining for the primary care practices would be 60% lower than they receive today.
- If the primary care practices can change care for their patients in a way that reduces the services delivered by specialists and hospitals by 4% (i.e., slightly more than the discount assumed in calculating the global payment), the amount remaining for the primary care practices would be 16% higher than what they are receiving today.
- However, if the number of services delivered to the patients by specialists and hospitals increase by 3%, there would be no money left at all to pay the primary care practices, and they would also have to pay Medicare $85 per patient to cover the amount by which total spending exceeded the global payment amount. If a practice had 250 Medicare patients, it would have to pay CMS $21,250 ($85 x 250).
FIGURE 33
Changes in Primary Care Practice Revenues Under Global Payment/Direct Contracting
| Current Spending Per Patient |
Global Payment |
Change From Current |
Reduction in Non-Primary Care Spending |
Change From Current |
Increase in Non-Primary Care Spending |
Change From Current |
||
|---|---|---|---|---|---|---|---|---|
| Payments | $10,000 | $9,700 | -3% | $9,700 | -3% | $9,700 | -3% | |
| Payments to Specialists/Hospitals | $9,500 | $9,500 | 0% | $9,120 | -4% | $9,785 | +3% | |
| Primary Care Revenue | $500 | $200 | -60% | $580 | +16% | ($85) | -117% | |
| Total | $10,000 | |||||||
Figure 34 compares how primary care practices would be paid under a global payment or direct contracting model if a group of primary care practices formed a Direct Contracting Entity or ACO and how they would be paid under Patient-Centered Primary Care Payment.
FIGURE 34
Comparison of Global Payment and
Patient-Centered Primary Care Payment
|
Payments for Primary Care Services Under Global Payment/Direct Contracting |
Payments for Primary Care Services in Patient-Centered Primary Care Payment |
|---|---|
| The primary care practice receives a monthly payment for each patient instead of payments for individual services. The amount of payment is risk-adjusted based on the patients’ chronic conditions in the previous year, but not based on any newly diagnosed chronic conditions or acute illnesses or injuries during the current year. | The primary care practice receives monthly payments for wellness care and chronic condition management for each patient, and fees for diagnosis and treatment when patients experience new acute problems. As a result, the practice receives higher payments for both new and pre-existing chronic conditions and also if multiple new acute problems occur during the year. |
| The primary care practice will initially receive less revenue that it has in the past, because the global payment is specifically set at a lower amount than was spent on patients in the past, and the primary care practice only receives what is left after all other providers are paid. | The payments the practice receives are set at levels that are expected to be adequate to cover the costs of delivering the services patients receive. |
| The primary care practice will receive an increase in revenue if it finds a way to reduce spending on specialists and hospitals, but the increase in revenue may or may not be large enough to cover any additional costs the primary care practice incurred to deliver additional services. | The payments the practice receives are set at levels that are expected to be adequate to cover the costs of delivering its services. The payments do not depend on how many services the patients receive from specialists or hospitals. |
| The primary care practice can receive higher revenues if it reduces spending by failing to deliver or order evidence-based services. | The practice is not paid unless it delivers or orders all appropriate, evidence-based services. |
| The primary care practice would receive less revenue if following evidence-based guidelines caused total spending on the patients to increase. | The practice is paid adequately for delivering and ordering all appropriate, evidence-based services, even if that causes total spending on the patients to increase. |
Predictability of Revenues Under Different Payment Systems
The Risks of Fee-for-Service Payment
From the primary care practice’s perspective, there is an additional problem with fee-for-service payment systems that has not been discussed in previous sections – the unpredictability of the practice’s revenues. Most of the costs of operating a primary care practice are very regular and predictable – the salaries and health insurance for the physician and staff, the rent for the office space, and the leases on equipment and software. However, the revenues for the practice depend entirely on how often patients have office visits with the physician. The practice can attempt to fill the physician’s schedule with as many visits as possible, but if the patients do not get sick or choose not to come to the practice when they are sick, the practice will lose money.
Although many people have been led to believe that providers have no “downside risk” under fee-for-service systems, they clearly have significant downside risk, since almost all of their costs are fixed in the short run, but all of their revenue depends on how often their patients get sick and whether they come to the primary care practice for services.
The magnitude of the financial risk associated with this unpredictability in revenues became particularly apparent during the coronavirus pandemic in 2020, when patients suddenly stopped making visits to primary care practices and other healthcare providers. Primary care practice revenues plummeted but the costs of operating the practices did not decrease, since salaries, rent, and other expenses still had to be paid. Many primary care practices were already operating on thin financial margins, so the reductions in revenue caused significant financial losses, and unlike non-profit and institutional healthcare providers, primary care practices did not have financial reserves that could enable them to continue paying their bills without any source of revenue.
The Uncertainties and Risks of Population-Based Payment
Since population-based payments are not tied to office visits or other services, it might appear they would provide the most predictable revenue stream for primary care practices and do the best job of avoiding the kinds of financial problems that occurred during the pandemic. However, in reality, population-based payment systems are not as predictable as they may seem due to at least four components that are typically included in those systems:
- Patient Attribution. In most population-based payment systems, patients do not need to enroll with the primary care practice and there may not even be a way (or an easy way) for them to do so. Instead, the patient’s health insurance plan determines whether to “attribute” the patient to a primary care practice based on a calculation of how often the patient has visited that primary care practice compared to other practices. It is impossible for a primary care practice to predict how many or which patients will be attributed to it because of the many errors that are inherent in the attribution methodology, i.e., patients can be receiving care from a primary care practice but not be attributed to it, and patients can be attributed to the practice even if they do not want to receive care there. For example:
- A new patient will not be attributed to the primary care practice until after the patient has made more visits to the new practice than they made to their previous primary care practice during the “lookback” period the health plan uses for the attribution methodology. For example, if attribution is determined annually, and if a patient makes 3 visits to their former primary care practice during January through June and then switches to a new primary care practice in July, the patient will not be attributed to the new practice until the following year and then only if the patient made at least three visits to the new practice between July and December. The first primary care practice will continue to receive monthly payments for the patient from July to December, even though the patient is no longer receiving services from the practice, and it may even continue to receive monthly payments the following year if the patient did not visit the new practice often enough during the second half of the year to trigger a change in the attribution formula.
- If a primary care practice is able to use the monthly population-based payments to deliver the services a patient needs without the patient having to come to the practice for an office visit, or if the patient remains healthy and doesn’t need to make an office visit, the patient may no longer be attributed to the practice, since attribution is based on where they make office visits. The health plan has no way to know what services the patient may be receiving if the services are not part of a billable office visit. In both the Comprehensive Primary Care Initiative and the Comprehensive Primary Care Plus demonstrations, a majority of primary care practices’ patients were not attributed to them.96
- Leakage Penalties. Even if the patient is attributed to the practice, the monthly payment amount the practice receives may be reduced if the patient receives primary care services from a different practice. For example, the CMMI Primary Care First payment model includes a “leakage adjustment” that reduces the Professional Population-Based Payment (PBP) in direct proportion to the number of primary care office visits the patients made to other practices. This calculation is based entirely on how many traditional office visits are delivered, so if a primary care practice delivers care in a way that is less dependent on traditional office visits, any visits its patients make to other practices for any reason (e.g., while they are visiting family in a different part of the country) could represent a significant proportion of the patients’ total visits, particularly for relatively healthy patients, and the payments to the primary care practice could then be reduced significantly. One study found that adjustments in payments to primary care practices based on whether patients made visits to other practices or an Emergency Department simply penalized those primary care practices that had more high-need patients.97
- Risk Adjustment. The risk scores assigned to patients in commonly-used risk adjustment systems do not reflect the differences in the time required to deliver primary care services. In addition, however, the risk scores are assigned by the health insurance plan based on diagnoses assigned to the patient during a prior year or prior period of time. It may be impossible for the primary care practice to predict what risk scores will be assigned to its patients, which means it is also impossible to predict what its payments will be.
- Performance-Based Payments/Adjustments. In most performance-based payment systems, the performance of the primary care practice depends not only on what it does, but on what other primary care practices do, what other providers do, and other events that are completely beyond the control of the primary care practice whose performance is being assessed. For example, in the CMMI Primary Care First payment model, the principal factor determining the Performance-Based Adjustment is a comparison of the rate at which the patients in the practice are hospitalized (for any reason) with the hospitalization rates for patients who are not part of the practice. The hospitalization rate for any group of patients is affected by many factors other than primary care services, and analyses have shown that the majority of hospital admissions are not in categories considered to be potentially preventable98, so it would be impossible for a primary care practice to predict how much of a Performance-Based Adjustment it would receive during the year. Random factors affecting the need for hospitalizations would likely result in significant variations in practice revenue from year to year.
Each of these factors will cause unpredictability and variability in the revenues a primary care practice will receive under population-based payments, and in combination, the unpredictability and variability in revenues could be as large or larger than under current fee-for-service systems. As a result, a primary care practice will still experience significant financial risk in population-based payment systems, even if the payment amounts might appear to be adequate to cover the practice’s costs. Moreover, all of the factors listed above are still tied in some way to the number of services that patients receive, so any significant change in the types of services that patients are able to receive, such as during a pandemic, could have a significant impact on the primary care practice’s revenues.
The Predictability of Patient-Centered Primary Care Payment
Under the Patient-Centered Primary Care Payment system, the practice would bill for and be paid the monthly Wellness Care Payments and Chronic Condition Management Payments for each patient who enrolled with the practice to receive those services, and the patient could remain enrolled whether they had a visit with the physician or not. The practice would know exactly how much revenue it would receive from these payments because it would know how many patients it had enrolled; it would not need to wait to see how many patients were attributed to it through a health plan’s calculation that could easily be affected by changes in the number and types of services patients were receiving.
During a pandemic or other public health emergency, the primary care practice would be expected to continue delivering wellness and chronic care management services where it was feasible to do so, and the monthly payments would provide the flexibility to do that through telehealth or other approaches when possible, but the practice would not be penalized if a patient failed to receive preventive care services or tests that would have to be delivered in person and could not be delivered due to safety concerns or if patients were hospitalized due to a natural disaster or an infectious disease in the community.
Even though a significant portion of a practice’s revenues under Patient-Centered Primary Care Payment would still be based on fees for addressing acute care problems, the fees would not be tied to in-person visits with the physician; the physician and other practice staff would have the flexibility to address acute care problems through telehealth or other methods that are feasible for the practice to safely deliver to patients during a pandemic, and the practice would be paid for those services. The biggest losses for primary care practices in 2020 occurred in the initial months of the pandemic before Medicare and other payers made payments available to support telehealth services and before primary care practices could gear up to begin delivering those services. These gaps in services and losses of revenue would never have occurred if Patient-Centered Primary Care Payment had been available to primary care practices.
Ensuring Access to Care for Disadvantaged Populations
The Strengths and Weaknesses of Fee-for-Service for Disadvantaged Patients
An important strength of fee-for-service payment is that if a patient needs more services, the primary care practice will be paid more to deliver those services. Patients who have many health problems, whether they be chronic or acute, may need to visit the primary care practice frequently, and under standard fee-for-service payment systems, the practice will be paid for each of those visits.
However, many patients not only need more visits, they also need much more time during and after these visits than a primary care practice can afford to provide because of the inadequate amounts currently paid for office visits. Moreover, it may be very difficult for patients to come to the practice office for a visit if they have limited mobility, if they do not have access to transportation, if they cannot afford to take time off of work, etc. Since fees have traditionally only been paid for office visits with a physician, these patients will not be able to receive the care they need. Although paying fees for home-based telehealth services is helpful, it will not solve the problem for individuals who do not have a computer or smartphone, who do not have access to affordable broadband services, or who need more time than in a typical telehealth visit.
Why Population-Based Payments and Medical Home (Hybrid) Payments Can Harm Disadvantaged Patients
Population-based payments and medical home (hybrid) payment systems can actually make these problems worse, not better:
- Population-based payments do not provide higher payments for patients who have new health problems, have multiple acute health problems, or who require more time or services due to non-medical factors. Population-based payments are typically risk-adjusted based only on the number and types of chronic diseases recorded for a patient during the previous year.99 There is no increase in the payment even for a patient who:
- has multiple acute health problems during the year;
- is diagnosed for the first time with a chronic disease;
- has difficulty using standard medications or treatments or requires more time or assistance to do so.
- Performance-based payments penalize primary care practices that have disadvantaged patients. Performance-based payments do not address any of the weaknesses in fee-for-service payments. They are focused on rewarding or penalizing primary care practices based on measures of the proportion of patients who have received specific services and/or achieved a particular outcome. Low-income patients may not be able to afford or access the medications and services required to achieve good outcomes, and some patients may have comorbidities or other characteristics that make it inappropriate for them to receive recommended services or difficult for them to achieve the outcomes required by the quality measures.100 There is generally no mechanism for a primary care practice to exclude these patients from the measures or to adjust the definition of “quality” to accommodate a patient-centered approach to care. There is no mechanism for adjusting measures of average spending or utilization based on the number of patients who have low functional status, limited access to community services, and other types of disadvantages.101 Consequently, the more disadvantaged patients a practice treats, the more likely it will have a lower score on quality and spending measures and be penalized financially as a result.102
How Patient-Centered Primary Care Payment Would Improve Care for Disadvantaged Patients
Patient-Centered Primary Care Payment would solve the problems with current fee-for-service payment systems and improve access to quality care for disadvantaged patients in three ways:
- Higher Payments for Patients With Multiple Acute Problems. For patients who experience frequent acute care problems, the primary care practice would be paid an additional fee for addressing each of those problems, similar to the current fee-for-service system. However, unlike current fee-for-service payments:
- The payment would be high enough to allow the practice to spend adequate time with the patient, and higher amounts would be paid for patients who need significantly more time during a visit.
- The payment would be flexible enough to allow the practice to address the patient’s needs in whatever way will work most effectively, whether by telephone, telehealth, or a face-to-face visit.
- Higher Payments for Patients With Complex Conditions. The practice will receive a higher monthly payment for those patients who have characteristics that require the practice to spend significantly more time managing care of a chronic condition. The higher payment is not based on how many diseases the patient has been diagnosed with, but based on the complexity of providing appropriate care for the patient.
- Accountability and Flexibility to Deliver the Most Appropriate Care for Each Patient. In return for adequate payments, the primary care practice would be accountable for delivering (or at least attempting to deliver) the care to each patient that is most appropriate for that specific patient. The practice would have the flexibility to deliver different services if they are necessary or appropriate given a patient’s unique needs, and the practice would not be penalized if a patient is unable or unwilling to use the recommended services.103
Summary of Patient-Centered Primary Care Payment vs. Other Systems
Figure 35 summarizes the extent to which Patient-Centered Primary Care Payment and other payment methods have characteristics that are desirable for a primary care payment system.
Figure 36 summarizes the extent to which Patient-Centered Primary Care Payment and other payment methods have characteristics that are problematic for a primary care payment system.
FIGURE 35
Desirable Characteristics of Primary Care Payment
| Desirable Characteristics of a Payment System |
Patient- Centered Primary Care Payment |
Current Fee for Service Payment |
Population- Based Payment/ Capitation |
Pay for Performance on Quality Measures |
Medical Home Payment Models |
Shared Savings ACOs |
Global Payment/ Direct Contracting |
|---|---|---|---|---|---|---|---|
| The primary care practice is paid for delivering proactive care and non-visit-based services as well as in-person office visits with a physician | YES | NO | YES | NO | YES | NO | YES |
| The payment amounts are set at levels expected to be adequate to cover the costs of delivering high-quality care | YES | NO | NO | NO | NO | NO | NO |
| Each patient is assured of receiving appropriate, high-quality care in return for payment | YES | NO | NO | NO | NO | NO | NO |
| The primary care practice receives additional resources and flexibility to help patients who have higher-than-average needs or face barriers in accessing services | YES | NO | NO | NO | YES | NO | NO |
FIGURE 36
Undesirable Characteristics of Primary Care Payment
| Undesirable Characteristics of a Payment System |
Patient- Centered Primary Care Payment |
Current Fee for Service Payment |
Population- Based Payment/ Capitation |
Pay for Performance on Quality Measures |
Medical Home Payment Models |
Shared Savings ACOs |
Global Payment/ Direct Contracting |
|---|---|---|---|---|---|---|---|
| Financial penalty for keeping patients healthy | NO | YES | NO | NO | YES | YES | NO |
| Financial penalty for delivering or ordering all services that patients need | NO | NO | YES | NO | YES | YES | YES |
| Financial reward for withholding needed services | NO | NO | YES | NO | YES | YES | YES |
| Financial penalty if spending increases or a patient experiences a poor outcome for reasons beyond the control of the primary care practice | NO | NO | YES | YES | YES | YES | YES |
Benefits and Costs of Patient-Centered Payment
Improvements in Care Delivery Under Patient-Centered Primary Care Payment
As discussed in Section 2, the current fee-for-service payment system not only fails to pay adequately for many services, it does not pay at all for many types of services and for methods of delivering services that may be more effective for individual patients than the services that are paid for. By correcting both of these problems, Patient-Centered Primary Care Payment will allow primary practices to significantly redesign the way they deliver care to patients.
Vignettes illustrate how much differently and more effectively preventive care, minor acute care, chronic disease care, and behavioral health care can be delivered by a primary care practice to different types of patients when the practice is paid using Patient-Centered Primary Care Payment. These examples make it clear why patient outcomes can be expected to improve significantly when the payment system is changed.
The Impact of Patient-Centered Primary Care Payment on Primary Care Spending
Increases in Medicare Spending on Primary Care
It is clear from the analyses in Sections 4 and 5 that the amount currently paid for primary care services under Original Medicare is not adequate to support the delivery of appropriate, high-quality primary care services to Medicare beneficiaries. As shown in Figure 31, a hypothetical primary care practice that was paid for office visits at Medicare’s rates in 2020 would only receive about half the revenue it needs to cover its costs. Although Medicare payments for office visits were increased by about 10% in 2021, these higher amounts will still be far less than what is needed to support high-quality primary care.
Based on the analyses shown in Sections 4 and 5, Medicare will likely need to spend about twice as much per beneficiary on primary care services in order to provide adequate payments for primary care. As shown in Figure 31, the Patient-Centered Primary Care Payment amounts required to cover the costs of primary care for Medicare beneficiaries would generate about twice as much revenue as standard Medicare payments.
Although doubling spending on primary care sounds very expensive, estimates indicate that only 4-5% of total Medicare spending currently goes to primary care practices.104 As a result, doubling the amount Medicare spends on primary care would require a 4-5% increase in total Medicare spending.
Moreover, Medicare is already increasing primary care spending by similar amounts in its primary care payment demonstration programs. Figure 31 shows that Medicare spending increases in Track 2 of CPC+ and in the new Primary Care First program are similar to the spending increase that would occur under Patient-Centered Primary Care Payment. However, as discussed in Section 5, both the amount and method of payment are important, and it would be far better for primary care practices to receive the increase in revenue they need through Patient-Centered Primary Care Payment rather than be paid through either the CPC+ or Primary Care First approaches.
Changes in Spending on Primary Care by Other Payers/Purchasers
Original Medicare pays essentially the same amount for the same service to every primary care practice in a community. This is not true for private health plans (including Medicare Advantage plans and Medicaid managed care plans):
- Two different health plans will pay two different amounts for the same service even when it is delivered by the same practice. Some health plans pay a primary care practice significantly more than Medicare rates for primary care services, and some pay significantly less.
- An individual health plan generally pays different amounts for a service depending on which primary care practice delivers the service, even though the service is the same. For example, many health plans pay significantly more than Medicare rates to large primary care practices and significantly less than Medicare rates to small primary care practices.
- Different health plans have different cost-sharing requirements for primary care services, so patients with similar needs may use primary care services at different rates depending on which health plan provides their insurance.
Under Patient-Centered Primary Care Payment, primary care practices would receive adequate support for their services if every payer paid the same amount for each service to all primary care practices in the community. Specifically:
- every health plan could pay the primary care practice the same amount for wellness care services for each of that plan’s members who enrolled with the practice for wellness care;
- every health plan could pay the practice the same amount to address an acute problem experienced by one of that plan’s members;
- every health plan could pay the practice the same amount for each member of the plan who has a chronic health condition and who enrolled with the practice to receive chronic condition management services; and
- every health plan would need to pay for wellness care and chronic condition management without patient cost-sharing and set cost-sharing amounts for acute care visits at affordable amounts.
The payments can be payer-agnostic because they are explicitly patient-centered, i.e., the payments are designed to support the time required to deliver the specific types of services each patient needs, and the amount of time needed for an individual patient does not depend on what kind of insurance they have. Moreover, the primary care practice should be able define the size of its patient panel based on the amount of time it would need to provide good care to the patients based on the health needs of those patients, not based on what kinds of insurance they have.
Although the payment for each service under Patient-Centered Primary Care Payment could be the same for every payer, the total amount spent on primary care would differ by payer because of the differences in the characteristics of the patients insured by different payers and purchasers. For example, Medicare will ordinarily spend more per beneficiary for primary care services than most commercial insurance plans will spend for each of their members because Medicare beneficiaries are more likely to have chronic conditions and to experience acute problems than the younger, healthier patients typically insured by commercial plans. However, under the Patient-Centered Primary Care Payment system, the higher spending per Medicare beneficiary compared to younger patients would be due solely to the differences in the needs of the patients, not because Medicare paid more for individual services.
If two different health plans in a community had members with similar health needs, or if two different employers had employees with similar health needs, each health plan or employer could expect to spend similar amounts on primary care services for those patients under Patient-Centered Primary Care Payment. However, because of the differences in the amounts they currently pay for primary care services, the change in spending on primary care services under Patient-Centered Primary Care Payment will differ significantly for different payers and purchasers:
- Spending on primary care services might change very little or even decrease for a health plan that currently pays significantly more than Medicare rates and encourages its members to use primary care services frequently, because the fees are already closer to actual costs, and under the Patient-Centered Primary Care Payment system, the primary care practices would likely be able to provide better care with even fewer visits than the patients are making today since the practices’ revenues would no longer be completely tied to the number of visits their patients make.
- On the other hand, spending on primary care services could more than double for a health plan that currently pays less than Medicare rates or if it has cost-sharing requirements that discourage patients from using primary care services. The more that a payer is underpaying for primary care today, the greater the increase it will need to make in the amount it spends on primary care.
For self-insured employers and other purchasers, the changes in primary care spending could be either larger or smaller than what other purchasers experience, even if their employees have similar health characteristics and even if they use the same health plans to administer their benefits, because the amount each purchaser is currently spending depends on the specific primary care practices their employees/beneficiaries use and how much those specific practices are currently paid for their services by the health plan(s) the employers are using.
Changes in Spending and Percentage of Spending on Primary Care Do Not Indicate the Adequacy of Primary Care Payments
This also means that the adequacy of primary care payments by a health insurance plan or purchaser cannot be evaluated by how much the payer increases spending on primary care. For example, if a health plan has been paying a primary care practice only 50% of Medicare fees, even if it doubles the amount it spends on services delivered by the practice, that will likely fall far short of what the practice needs to deliver high-quality care, regardless of what payment method is used. Conversely, if an insurance plan is paying relatively high fees for primary care today, its spending on primary care may need to increase by only a small amount or its spending may even decrease, but it needs to spend that money in a different way – using Patient-Centered Primary Care Payment rather than solely paying fees for traditional office visits.
The percentage of total healthcare spending that goes to primary care practice is also a poor indicator of the adequacy of primary care payment by a payer or purchaser, because the amount spent on primary care relative to the amount spent on other services depends on the characteristics of the patient population and the amounts paid for services to other providers as well as the amounts paid for primary care services. For example:
- For a relatively healthy group of individuals, a high proportion of the services they need could likely be delivered by a primary care practice, so a high percentage of total healthcare spending for this group would be expected to be used for primary care.
- A relatively unhealthy group of patients will likely need many services that cannot be delivered by a primary care practice, such as care from specialists and surgeries and treatments that have to be delivered in hospitals or other specialized facilities. For these patients, a large amount will need to be spent on these expensive non-primary care services, so even if a large amount is being spent on primary care, it will likely only represent a small percentage of total spending.
- A health plan that pays higher amounts than other plans for services delivered by specialists, hospitals, and other providers will spend more on those services even if its members are using those services at similar rates. That could cause the percentage of total spending on primary care services for that plan to be lower than other plans, even if the plan is paying primary care practices higher amounts for services than other payers.105
Because of this, it is both inappropriate and problematic to set targets for the percentage of total healthcare spending that primary care practices should receive. No matter what target amount is used, it may be too low or too high depending on the characteristics of the patient population and the community where they are receiving care. Moreover, if a payer implements other initiatives to reduce utilization rates or payment amounts for specialty services that cause total healthcare spending to decrease, this does not mean that payments for primary care should be reduced in order to maintain the same percentage spending.
Spending on primary care will only be adequate if the amounts paid for primary care services are sufficient to allow primary care practices to spend the time and hire the appropriate staff to deliver those services. That is the appropriate criterion for determining whether primary care payments are adequate, not the amount by which spending has changed or the percentage of total spending going to primary care.
The Impact of Higher Primary Care Payments on Total Healthcare Spending
Evidence indicates that total healthcare spending is lower in countries where individuals are able to receive high-quality primary care than in those where they are not able to do so.106 It is easy to see why this should be so – if the residents of a community cannot obtain good primary care, they will be more likely to have health problems that could have been prevented, they will be less likely to have health problems identified and treated early when treatment is less expensive and more likely to be successful, and the cost of many of the services they need will be higher if they are delivered by a hospital emergency department or other provider than by a primary care practice.
However, this does not mean that spending more on primary care for a specific group of individuals, such as the members of a health plan, the employees of a company, or the patients using certain primary care practices will reduce total healthcare spending for those individuals. In some cases, total spending will decrease, but in other cases, total spending will increase. This is because total healthcare spending for a group of individuals depends not just on the quality of the primary care services they receive, but also on the characteristics of those individuals, the ways that other (non-primary care) services are delivered and paid for, and the cost-sharing requirements for those services under their health insurance. For example:
- For a relatively healthy group of individuals, better access to higher-quality primary care could easily cause an increase in total healthcare spending, because a higher percentage of those individuals would likely receive screenings for cancer (e.g., colonoscopies and mammograms), and a higher percentage would use the medications they need to manage chronic conditions (e.g., medications to control cholesterol and blood sugar) and receive regular testing to monitor those conditions. Greater use of these services and medications is important for achieving better health outcomes for the patients, but the payments for these services will increase total healthcare spending, at least in the short run.
- A less-healthy group of individuals will likely be receiving multiple medications, more expensive medications, treatments from specialists, and/or hospital procedures. If some of these individuals are receiving tests, medications, or treatments that are inappropriate or unnecessary, the primary care practice may be able to help the patients avoid using these services, and this would reduce overall spending. However, if the patients are currently receiving appropriate and necessary treatments, the primary practice cannot and should not do anything to prevent patients from receiving them; moreover, primary care physicians may determine that some patients need additional specialty care services in order to more effectively address their problems, and helping the patients get appropriate care could increase total spending.
- If the prices of medications increase, or if the health plan increases the amounts it pays for tests, specialty care, or hospital procedures, then even if patients receive fewer of those services, total spending on the patients could increase.
The goal of primary care is to improve patients’ health, not to reduce healthcare spending. Since many patients currently receive poor quality primary care, unnecessary specialty services, and unnecessarily expensive treatments, improving the quality of primary care will likely result in some reduction in spending on other kinds of services for many groups of patients. However, for the reasons described above, one cannot assume that these savings will completely offset the increase in spending needed to provide adequate support for primary care.
If total spending on the patients in a primary care practices decreases, it does not necessarily mean that the primary care practice is delivering good care to those patients. Conversely, an increase in total spending does not in and of itself indicate that the primary care practice is doing a poor job. Unfortunately, many efforts ostensibly designed to improve payments for primary care have made the payments explicitly or implicitly contingent on whether there is a reduction in total healthcare spending on the patients in a primary care practice. For example:
- Many payers have implemented “shared savings” payments for primary care practices, in which the primary care practice receives higher payments only if there is a reduction in total healthcare spending for its patients. For the reasons described above, good primary care may result in an increase in total spending as well as a reduction, and total spending may increase or decrease for reasons that have nothing to do with the way primary care is delivered and that are beyond the control of a primary care practice. As a result, the primary care practice may receive little or nothing in terms of a shared savings bonus. If the primary care practice restructured its operations to provide better care to patients, the practice could lose money even if it does receive a shared savings payment, since the shared savings payment amounts are not designed to cover the costs of delivering high-quality care. Moreover, shared savings payment systems create a perverse financial incentive for a primary care practice to withhold ordering needed services from patients in an effort to avoid an increase in total spending or to receive a share of the savings that result when patients receive fewer services.
- Primary care payment initiatives and demonstration projects have been deemed successes or failures based on whether an evaluation shows there was a reduction in total spending on the patients. For example, even though the evaluations of Medicare’s Comprehensive Primary Care Plus demonstration have indicated that the quality of care increased and spending on non-primary care services decreased, the program is not being continued or expanded because the reductions in other spending were not large enough to completely offset the increases in primary care spending.
- In an effort to avoid increasing total spending, primary care payment initiatives provide payments that are too small to support the delivery of high-quality care. For example, CMMI is replacing CPC+ with the Primary Care First demonstration project, which (as shown in Figure 31) does not pay adequately for primary care services and also makes a large proportion of the primary care practice’s revenue contingent on things it cannot control. Since payments are inadequate, it is less likely that an evaluation of this new program will show improvements in quality or reductions in spending.
If total healthcare spending increases when primary care practices are paid adequately and are delivering high quality care, this does not mean the payments to primary care are too high or that there is not enough “incentive” for the primary care practice to reduce healthcare spending. It is more likely to mean that not enough is being done to change the way specialists and hospitals are paid or to provide information to primary care practices on the relative costs of different providers. Most of the primary care demonstration programs implemented by Medicare and other payers do nothing to change the way other providers are paid or to increase transparency about the cost of services the other providers deliver, yet the programs measure the success of the primary care practices based on whether spending on those other providers decreases.
Moreover, the calculations of “savings” used in evaluations and shared savings models implicitly assume that total spending will remain the same if spending on primary care does not increase. Inadequate payments for primary care are forcing many primary care practices to close and new physicians are being discouraged from entering the field. If access to primary care is significantly reduced, it is likely that spending on other services will increase, both in the short run and the long run. The correct “benchmark” for calculating changes in spending is not the current level of spending, but the higher spending that would result if access to high-quality primary care services continues to decline. However, since it is impossible to know how much higher spending would be if access to quality primary care services continues to decrease, it is also impossible to accurately determine the true impact on total spending from paying adequate amounts for primary care.
The right way to evaluate a primary care payment model is by whether it has provided sufficient resources to cover the costs of delivering high-quality primary care services to every patient, and whether the accountability component ensures that every patient is receiving appropriate, high-quality care. Unfortunately, Congress required the Center for Medicare and Medicaid Innovation (CMMI) to focus on projects that will reduce total Medicare spending. Moreover, CMMI is prohibited from continuing or expanding a demonstration project unless the CMS Office of the Actuary certifies that total spending will not increase, and as a practical matter, the Actuary will never certify a CMMI model unless an evaluation shows that it actually reduced total Medicare spending.
Consequently, unless Congress changes the statute, it is unlikely that CMMI would ever implement a demonstration program using Patient-Centered Primary Care Payment or any other payment model that provides adequate support to primary care.
The Economic Value of Better Health and More Patient-Centered Service Delivery
While too much weight has been placed on the impact of primary care on total healthcare spending, too little weight has been placed on the beneficial impacts effective primary care can have on worker productivity. Working-age individuals who have poorly managed chronic conditions or who have untreated or improperly treated acute health problems are likely to either be completely absent from work or to have what is often called “presenteeism,” i.e., the individual is on the job but is not functioning efficiently or effectively. Analyses have estimated that for many types of common health problems, the cost of lost productivity from both absenteeism and presenteeism is much greater than the amount spent on healthcare services to treat them.107
Many of the health problems that have the biggest impacts on worker productivity can be effectively treated or managed by primary care practices if they have the time and resources to do so. If workers stay healthy and if they can have their health issues addressed effectively without having to make multiple visits to different physicians, they will spend less time away from work and be more productive when they are working.
Patient-Centered Primary Care Payment can help primary care practices improve worker productivity in several different ways:
- The primary care practice will be organized to respond quickly when a patient has a new health problem or an exacerbation of an existing problem, rather than forcing a patient to suffer with symptoms for days or even weeks before being diagnosed and treated.
- The primary care practice will have the flexibility and resources to provide services to patients in a way that is convenient for the patient’s work schedule and responsibilities. The patient will not be forced to miss work in order to come to the physician’s office for something that could have been addressed over the phone or through a telehealth connection, and the patient will not be forced to make multiple short visits to resolve what could be addressed in a single visit of adequate length.
- The primary care practice will be accountable for delivering the evidence-based services to each patient that are most likely to successfully address their health problems, and it will have adequate time and staff to help patients understand and successfully use those services.
- The primary care practice will also be accountable for monitoring how well patients are doing so it can modify treatments (or diagnoses) when the initial evidence-based services are not working well for a particular patient.
Unfortunately, most evaluations of improved payments for primary care have not even examined the impacts better primary care services have on worker productivity. This is because (1) many of the evaluations have focused primarily on Medicare beneficiaries, most of whom are not working, (2) the measure of success is defined as reductions in healthcare spending or compliance with quality measures, not the ability of patients to work, and (3) it is far easier to measure changes in healthcare spending than changes in worker productivity. Of course, if a primary care payment reform does not provide payments that are large enough or flexible enough to allow care to be delivered in significantly different ways, it is unlikely that an evaluation would find large impacts on worker productivity even if they were measured.
Higher worker productivity has a direct economic benefit for employers, both by reducing costs (e.g., avoiding the need to hire temporary workers) and increasing revenues (through the ability to deliver more products or services). The resulting higher profits experienced by the employer will offset at least some and potentially all of the higher amounts spent to support high-quality primary care services for its employees. The employees also receive an economic benefit: hourly workers will have higher incomes if they miss fewer hours of work, and employees can be paid more if they increase the profitability of their employer.
The monetary benefits of higher productivity may well offset any net cost of higher primary care. However, the benefits of higher productivity accrue to the employer and employees, not to the employees’ health insurance plan. The cost of higher spending on primary care will be passed on directly to self-insured employers, but for small businesses and individuals that purchase health insurance directly, higher spending for primary care will need to come out of the premiums collected by the health insurance companies. The benefits of improved productivity for the small businesses and workers would help to offset any increase in insurance premiums they might need to pay.
Implementing Patient-Centered Primary Care Payment
Three sets of actions will be needed to implement Patient-Centered Primary Care Payment:
- The parameters for billing and payment of primary care practices must be defined.
- The clinical guidelines and related tools must be available to ensure that appropriate, high-quality care is delivered.
- Payers must implement the changes in payments for primary care practices and cost-sharing requirements for patients.
Operationalizing Billing and Payment
Two actions will be needed in order to enable primary care practices to bill and be paid for primary care services under Patient-Centered Primary Care Payment: (1) creating billing codes for the services primary care practices will deliver, and (2) assigning adequate payment amounts to those billing codes.
Creation of Billing Codes and Rules
As discussed in Section 4-B-2, for patients who have insurance coverage, the primary care practice would be paid by submitting a claim form each month to the patient’s health insurance plan. The claim form would include the codes for one or more of the new payments in Patient-Centered Primary Care Payment (i.e., the monthly Wellness Care Payment, the Acute Care Visit Fee, etc.) when the practice has delivered the services associated with those payments to the patient during the month.
Ideally, these codes should be part of the standard set of CPT® (Current Procedural Terminology) codes that describe the services physicians deliver. The American Medical Association’s CPT Editorial Panel should establish a formal definition for each of the patient-centered primary care services (e.g., a month of Wellness Care) and assign a specific CPT code to that definition.
Many people mistakenly believe that because CPT codes are the basis of payment in the current fee-for-service payment system, CPT codes cannot be used for different methods of paying for services, such as monthly payments or bundled payments. However, there are currently CPT codes for certain kinds of monthly and bundled services (e.g., CPT Code 99490 is used to pay for a month of chronic care management services, and CPT Codes 90951-90966 are used to pay for a month of services to patients with End Stage Renal Disease), so there is no reason why CPT codes cannot be created for each of the services/payments under Patient-Centered Primary Care Payment.
Although there are some existing CPT codes that are similar to some of the service concepts in Patient-Centered Primary Care Payment, an important principle of the CPT system is that physicians should only use a code if they have delivered the service that is specifically defined in the code, and they should not use a code for a service that is merely similar to the service they have actually delivered. The services described in Section 4 are different from the services described in current CPT codes, so current CPT codes could not be used. For example, the current CPT code for Chronic Care Management (CPT Code 99490) is only applicable to patients with two or more chronic conditions that place the patient at significant risk of death, acute exacerbation, or functional decline and the patient must receive at least 20 minutes of clinical staff time during the month, whereas the monthly Chronic Condition Management code in Patient-Centered Primary Care Payment (“XX031”) would include patients with one chronic disease and it would require the delivery of all appropriate evidence-based services to the patient, not simply that a specific amount of time was spent on the patient’s care.
When the CPT Editorial Panel creates a new code, it also specifies whether there are any other CPT codes that should not be used for the same patient during the same period of time. These rules are then incorporated into the National Correct Coding Initiative (NCCI) Procedure-to-Procedure (PTP) Column One/Column Two Correct Coding edit file108 to ensure a claim containing the ineligible codes would not be paid. For example, under Patient-Centered Primary Care Payment:
- a practice that bills for services using the codes for Wellness Care, an Acute Care Visit, and Chronic Condition Management should not also bill for services using existing Evaluation and Management Services CPT codes for Office or Other Outpatient Visits with Established Patients (CPT codes 99211, 99212, 99213, 99214, and 99215) or for Chronic Care Management Services (CPT codes 99490, 99487, and 99489).
- on the other hand, the practice should be able to continue billing for other Evaluation and Management Services codes when appropriate; for example, the CPT codes for Initial Hospital Care (99221-99223) and Subsequent Hospital Care (99231-99233) would still be used if the physician is managing the care of a patient during a hospital stay.
Temporary Billing Codes Until CPT Codes Are Created
If the new CPT codes have not been established by the time a payer is willing to begin using Patient-Centered Primary Care Payment to pay a primary care practice, the practice could begin billing using a combination of two types of existing codes:
- Unlisted” service CPT codes. There are a number of CPT codes that exist for the explicit purpose of allowing physicians to bill for delivering a service that is not accurately described by any other CPT codes. For example, CPT code 99499 is for an “Unlisted evaluation and management service” and CPT code 99429 is for an “Unlisted preventive medicine service.”
- Existing HCPCS Codes. There are a number of “G-codes” (so named because the codes all begin with the letter G) in the Healthcare Common Procedure Coding System (HCPCS) that have been created to allow Medicare payments for services that are not described by CPT codes. Some of these G-codes are used routinely to pay for services for any Medicare beneficiary, while others are used only in Medicare demonstration programs. There are a number of G-codes that were created for use in demonstration programs that are no longer operational and could be re-purposed for implementation of Patient-Centered Primary Care Payment, such as the G9001-G9012 codes that were created for use in the Medicare Coordinated Care Demonstration. There are also a series of “S-codes” that were created for use by private payers and “T-codes” that were created for use by Medicaid programs that could be used for Patient-Centered Primary Care Payment, such as S0281 (Medical home program, comprehensive care coordination and planning, maintenance of plan), S0311 (Comprehensive management and care coordination for advanced illness, per calendar month), and T2023 (Targeted case management, per month).
The payer and the primary care practice would simply need to agree (as part of their payment contract) which code the practice will use to bill for each of the services in Patient-Centered Primary Care Payment and the amount the payer will pay for a claim with each code. For example, Figure 37 shows codes that could be used temporarily for each of the payments in Patient-Centered Primary Care Payment.
Once the permanent CPT codes are established, the primary care practice would begin using those codes instead of the unlisted CPT codes and G-codes.
FIGURE 37
Temporary Billing Codes for
Patient-Centered Primary Care Payment
| Permanent Code |
Patient-Centered Primary Care Service |
Temporary Code |
|---|---|---|
| XX010 | Wellness Care (Monthly) |
99429 (Unlisted preventive medicine service) |
| XX011 | Transitional Care Management (Month) |
99199 (Unlisted special service) |
| XX012 | Integrated Behavioral Healthcare (Monthly) |
90899 (Unlisted psychiatric service or procedure) |
| XX020 | Acute Care Visit Fee (Per Event) |
99499 (Unlisted evaluation and management service) |
| XX030 | Initial Mgt of a Chronic Condition (Month) |
G9001 (Coordinated care fee, initial rate) |
| XX031 | Management of a Chronic Condition (Monthly) |
G9002 (Coordinated care fee, maintenance rate) |
| XX032 | Management of a Complex Condition (Monthly) |
G9005 (Coordinated care fee, risk adjusted maintenance) |
Assigning Adequate Payment Amounts
As discussed at length in Section 4, no matter how desirable the method of payment is, if the amounts of the payments are not adequate, a primary care practice will not be able to deliver high-quality care. Consequently, once the CPT codes for Patient-Centered Primary Care Payment are defined, an adequate payment amount needs to be assigned to each code.
The RBRVS System for Determining Payments for Physician Services
The amount that Medicare and most health plans currently pay for a service delivered by a physician is determined through a two-step process: (1) the CPT code for the service is assigned a Relative Value Amount (RVU) and (2) the RVU is multiplied by a Conversion Factor.
All current CPT codes are assigned a specific Work RVU (Relative Value Amount) that is intended to reflect the amount of time and effort that a physician needs to devote to delivering the service described by that CPT code relative to other types of services. The Work RVU is a ratio compared to other services, not an absolute measure such as hours; for example, an RVU of 1.5 means that the work involved for that service is 50% greater than a service with an RVU of 1.0.
Each CPT code is also assigned (1) a Practice Expense RVU to reflect the relative costs of staff, office space, etc. associated with delivering the service compared to other services, and (2) a Professional Liability Insurance RVU to reflect the relative cost of malpractice insurance for that type of service. These three RVU amounts are summed to determine the Total RVU for the CPT code. The RVU amounts for all of the CPT codes are collectively known as the Resource-Based Relative Value Scale (RBRVS).
In order to determine the actual dollar amount paid for each service, the RVU amount for each CPT code has to be multiplied by a Conversion Factor. The Conversion Factor can change from year to year based on inflation and other factors, and it can differ in different communities to reflect geographic differences in unit costs. Using a Conversion Factor allows the dollar amounts of all services to be uniformly adjusted for these factors, while using the RVUs ensures the payments for different services remain proportional to the differences in time and costs between those services.
How RVUs Are Assigned to Services
The RBRVS system was first used in 1992 to pay for physician services for Medicare beneficiaries. The initial RVU value for each CPT code was based on a study conducted by Harvard University, but since then, RVUs for new services and adjustments to the RVUs for existing services have been developed by the American Medical Association/Specialty Society RVS Update Committee, commonly known as the “RUC.” When the CPT Editorial Panel creates a new CPT code, the RUC develops a recommendation on the number of RVUs that should be assigned to that code. The RUC also reviews and makes adjustments to the RVU amounts for existing CPT codes when there is reason to believe they are no longer accurate.109
In most cases, the Centers for Medicare and Medicaid Services (CMS) uses the RVU values recommended by the RUC in determining Medicare payments, but it is not obligated to do so, and in some cases, it assigns a different number of RVUs to a CPT code than what the RUC has recommended.
How Conversion Factors Are Determined
The RUC’s role is limited to determining the appropriate number of RVUs for a service. The conversion factor used to convert the RVUs into a dollar amount of payment is established by each individual payer (i.e., Medicare or a health insurance plan).
In the Medicare program, the Center for Medicare and Medicaid Services (CMS) establishes a new conversion factor each year through regulation, using a methodology specified in statute. The Medicare conversion factor was originally supposed to be increased every year by an Update Factor designed to reflect inflation (as measured by the Medicare Economic Index). However, Congress now specifies the annual Update Factor in law, and it is no longer based on actual inflation amounts.110
Although the law requires the use of the RBRVS system in Original Medicare, there is no requirement for commercial health plans, Medicare Advantage plans, and Medicaid plans to use the system in determining the amounts they pay for services. Moreover, although Medicare uses the same conversion factor for all physician practices in the same community, private payers typically use different conversion factors for different physician practices, so they may pay very different amounts for the same service depending on which physician practice delivers that service.
The Cause of Inadequate Payments for Services Under RBRVS
Under the RBRVS system, the amount Medicare or a health insurance plan pays for a service can be below the cost of delivering that service either because the RVU value for the service is too low or because the conversion factor used by the payer is too low. Many people have inappropriately blamed inadequate payments for primary care services on the RVU values assigned to the services by the RUC111, when the problem has actually been caused by the conversion factors used by Medicare and other payers:
- The conversion factor used by Medicare is too low. No matter how accurate the RVU value is, if the conversion factor is too low, the resulting payment amount will not be adequate. The conversion factors that Medicare has used are too low for two reasons:
- Small Annual Updates. From 2016 to 2018, the Update Factor was only 0.5%, the Update Factor in 2019 was 0.25%, and beginning in 2020, the Update Factor is 0.0% (i.e., there will be no change at all in the conversion factor based on inflation).112 Since these updates are below the rate of inflation, the dollar amounts of payments for all physician services have decreased in real (i.e., inflation-adjusted) terms each year and will continue to do so. Moreover, since payment rates for services delivered in hospitals are not only higher but are increased each year based on inflation, the gap between the amount Medicare pays a physician practice vs. a hospital to deliver the exact same service increases every year.
- Budget Neutrality Requirements. Medicare spending on physician services is required by law to be “budget neutral.” This means that when new types of services are created or when the RVUs assigned to existing services are increased because more time or cost is required, the overall conversion factor will be reduced (or increased by a smaller amount than otherwise) in order to prevent total spending from increasing more than the annual update amount.113 A reduction in the conversion factor means that the payment for all services will be reduced. Because of this law, creation of a new surgical procedure means that the amount Medicare pays for primary care services will be reduced, and conversely, increasing the RVU values for primary care services, or paying for additional types of primary care services, will result in a reduction in payments for surgeries and other services. For example, in 2021, after the RUC recommended increasing RVU values for office visits significantly and CMS agreed to use the higher RVU values, CMS reduced the conversion factor by 10.2% to offset the higher spending that was expected to result from the higher RVUs. The result was that payments for office visits did not increase as much as the RVU values increased, and payments for surgeries and other procedures were reduced. As a result of both the low annual updates and the budget neutrality requirements, the Medicare Conversion Factor in 2021 is almost 9% lower than it was two decades earlier in 2001, even though the amounts that physician practices have to pay for staff, insurance, supplies, and office space have increased during that time.
- Payers other than Medicare use lower conversion factors for some primary care practices or do not use the RBRVS system at all. Health insurance plans that use RBRVS do not need to use the Medicare Conversion Factor and they frequently use different conversion factors for different physician practices. If a private health plan pays primary care practices using a lower conversion factor than it uses for specialty practices, the effect is the same as if the plan had reduced the RVU amounts for primary care services. Some payers use fee schedules for services that bear no relation to the RBRVS structure.
- Medicare and other payers do not pay anything for some primary care services, even when a CPT code and RVU amount has been assigned. The fact that there is a CPT code and RVU amount assigned to a service does not guarantee that Medicare or a health plan will actually pay for the service when it is delivered. For example, there have been CPT codes for evaluation and management services conducted by telephone since 2008 (99441-99443), and the RUC assigned RVUs to these codes when they were created, but the codes were not authorized for payment in Medicare until CMS changed the rules during the coronavirus pandemic in 2020. In effect, a Medicare conversion factor of $0 had been assigned to those services before 2020. Similarly, the CPT codes for evaluation and management services allow those services to be delivered through telehealth technologies rather than only in a physician’s office, but until 2020, Medicare and other payers would not pay if the services were delivered through telehealth to a patient in their own home.
Incorporating Patient-Centered Primary Care Payments Into RBRVS
Primary care practices will still bill and be paid for many current CPT codes under Patient-Centered Primary Care Payment (e.g., for procedures and for initial office visits with new patients). Rather than create a completely different approach for determining the appropriate amounts for the new payments under Patient-Centered Primary Care Payment, it would be desirable to use the RBRVS system.
- The American Medical Association/Specialty Society RVS Update Committee (RUC) should assign appropriate RVU amounts for each of the new CPT codes for Patient-Centered Primary Care Payment.
- Medicare and health insurance plans should use appropriate Conversion Factors to convert the RVUs for Patient-Centered Primary Care Payment CPT codes into adequate payments for participating primary care practices.
Setting the RVUs for CPT Codes in Patient-Centered Primary Care Payment
Initially, it will be impossible for the RUC (or anyone else) to determine exactly what RVU amounts are “right” for the Patient-Centered Primary Care Payment CPT codes. There is very little data on how much time and cost is involved in delivering the services because the current payment system prevents primary care practices from delivering services in the desired way. As shown in Section 4, one can estimate what the appropriate amounts might be, but then, after the services are being delivered, the amounts will need to be revised based on information about the actual time and costs required.
This is exactly the process that is currently used by the RUC to assign and update RVUs for all new CPT codes. When a new type of physician service is defined and a CPT code is assigned, the RUC engages in a process to estimate what the appropriate RVU for that service should be, using whatever data it can obtain and making informed assumptions in order to fill the gaps in data. After the service is being delivered, the RUC collects data on the actual time and costs involved and determines whether and how to revise the RVU value.
In fact, the RUC engaged in exactly this type of process for primary care in 2008 when it was asked by CMS to recommend RVUs for payments under a medical home demonstration project that was mandated by Congress.114 The RUC developed recommended RVU amounts for the types of payments CMS was planning to make by estimating the amount of time that physicians would need to spend carrying out additional medical home services for Medicare beneficiaries based on the types of services and the characteristics of the beneficiaries. The RUC also estimated the amount of time that nurses would need to spend providing services to the patients and the need for non-personnel resources such as an Electronic Health Record, in order to help determine what the Practice Expense RVUs should be.115
After the RUC establishes RVUs for the new Patient-Centered Primary Care Payment CPT codes, it can also re-examine the RVUs assigned to the existing CPT codes that primary care practices would continue to use, such as the payments for visits with new patients and delivery of procedures, to ensure the RVUs are adequate and appropriate in light of the changes in the patient panel sizes expected under the new payment system. If necessary, the RUC could recommend the creation of new CPT codes or modifiers to properly reflect the different ways that primary care practices deliver services or the different costs associated with services delivered in primary care practices.
Using an Appropriate Conversion Factor in Patient-Centered Primary Care Payment
As soon as estimates are made of the time and costs associated with delivering the services associated with the new CPT codes in order to assign the RVU amounts, the information on times and costs can also be translated into:
- an estimate of the optimal number of patients for whom a primary care practice could provide high-quality care;
- an estimate of the total number of RVUs for the new services the practice would deliver to those patients; and
- an estimate of the total amount of revenue that a primary care practice would need to receive to cover its costs for the services delivered to those patients.
These estimates could be made using calculations similar to those used in the simulations shown in Section 4.
The appropriate Conversion Factor can then be determined by dividing the estimated total revenue needed by the estimated total RVUs for the services that would be delivered, i.e., since the actual total revenue would be the sum of the RVUs times the Conversion Factor, the appropriate Conversion Factor would be the ratio of the total revenue needed and the sum of the RVUs.
These types of calculations are not typically carried out by the RUC, but the RVU values the RUC assigns will be of little benefit if they are not converted into adequate payment amounts. To address this:
- The American Medical Association/Specialty Society RVS Update Committee (RUC) should conduct or commission a special analysis to determine an appropriate conversion factor for Patient-Centered Primary Care Payment CPT codes. Many of the data and assumptions needed to calculate the RVUs would also be used to make the calculations required for the Conversion Factor.
- Alternatively, organizations such as the Patient-Centered Primary Care Collaborative or the Medical Group Management Association could carry out this analysis. The analysis could combine the data assembled by the RUC in setting the RVUs with information about the actual unit costs in practices, and be made publicly available for use by payers and purchasers.
The Conversion Factor that is needed is likely to be significantly higher than the standard Conversion Factor in Medicare because of the problems with the Medicare Conversion Factor described earlier. Consequently, for primary care practices receiving Patient-Centered Primary Care Payment, CMS will need to make an adjustment to the payment amounts that would be determined using its standard Conversion Factor. This will not be difficult to do, since CMS already makes a number of “policy adjustments” to the payment amounts calculated by multiplying RVUs by the standard Conversion Factor, including reductions for non-participating physicians, bonuses for physicians practicing in Health Professional Shortage Areas, and increases or decreases specified under the Quality Payment Program based on performance in the Merit-Based Incentive Payment System and participation in Alternative Payment Models. CMS also makes adjustments to the payments for certain services delivered by primary care practices that are participating in Track 2 of the Comprehensive Primary Care Plus demonstration. The adjustment needed for primary care practices receiving Patient-Centered Primary Care Payment would simply be an addition to this existing list of adjustments.
For private insurance plans, the Conversion Factor needed to create adequate payments may be higher or lower than what the plan is currently using for an individual primary care practice. If an increase is needed, the health plan could make an adjustment to the payments, similar to what is described for Medicare.
Using Temporary Payment Amounts Until RVUs Are Established
If the RVUs have not been determined by the time a payer wants to begin using Patient-Centered Primary Care Payment to pay a primary care practice, the payer and the practice could simply agree on the payment amounts that would be used for each billing code. The estimated payment amounts described in Section 4-D could be used as a starting point, with appropriate adjustments based on community-specific costs, etc.
If the RVUs have been determined but appropriate Conversion Factors have not been otherwise established, the estimated payment amounts described in Section 4-D could be divided by the RVUs to calculate initial Conversion Factors.
Operationalizing Accountability for Quality and Utilization
As explained in Section 4-C, in order to bill for one of the services in Patient-Centered Primary Care Payment, the primary care practice would need to deliver services to the patient consistent with a Clinical Practice Guideline (CPG), Clinical Pathway, or Standardized Clinical Assessment and Management Plan (SCAMP) that is appropriate for the patient or document the reasons for deviation. In particular:
- in order to bill for a monthly Wellness Care Management payment for a patient, the practice would need to have delivered or ordered wellness and preventive care services appropriate for that patient that are consistent with a CPG, Pathway, or SCAMP, or have documented the reasons for deviation. If the primary care practice also delivers integrated behavioral healthcare services, it could bill for a monthly Integrated Behavioral Healthcare Payment for each patient if it has carried out appropriate behavioral health screenings and any necessary interventions for patients consistent with a CPG, Pathway, or SCAMP, or it has documented the reasons for not doing so.
- in order to bill for a monthly Chronic Condition Management payment for a patient, the practice would need to have delivered or ordered services consistent with a CPG, Pathway, or SCAMP that is applicable to the patient’s chronic condition (or combination of conditions), or documented the reasons for deviation.
- in order to bill for an Acute Care Visit Fee for an individual patient, the practice would need to have delivered services to that patient that are consistent with a CPG, Pathway, or SCAMP that is appropriate for the patient’s acute problem or symptoms, or to have documented the reasons for deviation.
In addition, the primary care practice would need to use a Standardized Assessment, Information, and Networking Technology (SAINT) to identify and prioritize any problems the patient was experiencing in order to take actions to address those problems consistent with a CPG, Pathway, or SCAMP.
Using Existing Clinical Practice Guidelines/Pathways
Fortunately, Clinical Practice Guidelines already exist for most of problems and conditions commonly addressed by primary care practices and also for many less-common conditions, so this aspect of Patient-Centered Primary Care Payment can be implemented immediately. For example:
- Acute Back Pain: The Institute for Clinical Systems Improvement (ICSI) has developed guidelines for diagnosis and treatment of acute and subacute low back pain in adults.116
- Upper Respiratory Illness: The Institute for Clinical Systems Improvement (ICSI) has developed guidelines for diagnosis and treatment of respiratory illness symptoms.117
- Preventive Care: The United States Preventive Services Task Force (USPSTF) has developed recommendations for the types of screenings and preventive services appropriate for a wide range of different health conditions.118 In addition to the individual USPSTF recommendations, overall guidelines incorporating all of the recommendations have been developed.119
- Asthma: The National Asthma Education and Prevention Program Coordinating Committee has developed guidelines for the diagnosis and management of asthma.120
- Depression: The Institute for Clinical Systems Improvement (ICSI) has developed guidelines for diagnosis and treatment of adult depression in primary care.121
- Diabetes: The American Diabetes Association has developed a detailed Standard of Medical Care in Diabetes122, and the American Association of Clinical Endocrinologists and American College of Endocrinology have jointly developed a Comprehensive Type 2 Diabetes Management Algorithm.123
- Ischemic Heart Disease: The American College of Cardiology, American College of Physicians, American Heart Association, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons have jointly developed a set of guidelines for diagnosis and management of patients with stable ischemic heart disease.124
These and other guidelines have been developed by medical specialty societies and multi-stakeholder collaboratives in order to improve the accuracy of diagnosis and the effectiveness of treatment while avoiding the delivery of unnecessary services. The guidelines have been developed by groups of physicians, not by payers or manufacturers of specific drugs or tests, and strong efforts are made to ensure that the guidelines are based on what is best for patients.
Clinical Practice Guidelines vs. Quality Measures and Prior Authorization
An examination of any of these guidelines demonstrates that they provide a far more comprehensive and patient-centered way of assuring the delivery of high-quality care to every patient than the simplistic and problematic quality measures currently being used to evaluate primary care services. For example, the Glycemic Control Algorithm developed by the American Association of Clinical Endocrinologists and American College of Endocrinology explicitly indicates that the target level for HbA1c should be higher for patients with concurrent serious illnesses or who are at risk for hypoglycemia, that different treatments are appropriate depending on the patient’s HbA1c level when they began treatment, and that the appropriate initial treatment for patients who have an HbA1c level over 9.0% will depend on the nature of the symptoms that patient is experiencing.125 In contrast, in the HbA1c quality measure most commonly used by payers, the only thing that matters is whether the most recent HbA1c level is over 9.0%.
Moreover, most of the guidelines are specifically designed to avoid overuse of expensive services in a more patient-centered way than current payer-designed prior authorization programs. For example, the ICSI guidelines for acute back pain specifically identify the “red flags” that would warrant ordering an imaging study126, rather than treating all imaging studies as being inappropriate the way that prior authorization programs created by payers implicitly do. The guidelines for ischemic heart disease are specifically designed to avoid unnecessary use of cardiac stress testing, cardiac imaging, and cardiac catheterization, while also avoiding undertesting patients in a way that could lead to preventable heart attacks or death.127 In contrast, in a prior authorization process, an employee of a health insurance plan cannot possibly make good decisions about appropriateness of cardiac tests when they have not actually examined the patient or talked with them about the many different aspects of their symptoms and history that are required to make good clinical decisions.
Since use of the guidelines would achieve the stated goals of quality measurement and prior authorization programs more effectively than those programs do themselves, there is neither a need nor any benefit to have health insurance plans develop their own guidelines or to require the use of different guidelines. Indeed, it would be inappropriate for physicians to treat patients differently simply because of the type of insurance they have or to use guidelines that are designed primarily to save money for a health insurance plan rather than to ensure patients get the most appropriate care.
Facilitating Use of Clinical Practice Guidelines by Primary Care Physicians
Primary care physicians diagnose and treat a large and diverse set of problems and conditions. As illustrated above, Clinical Practice Guidelines exist for most of the symptoms and diseases that are commonly addressed by primary care practices and also for many less-common conditions. The guidelines for individual diseases are typically developed by physicians who specialize in treating that disease, although the guidelines are then used by primary care physicians as well as by specialists. Use of the same guidelines by both primary care physicians and specialists also helps to ensure coordinated approaches to care when both a primary care physician and a specialist are providing care to an individual patient.
As a result of this, however, the guidelines that primary care physicians would use will come from many different sources. Although it is not essential that every primary care practice use the exact same set of guidelines, it would be far easier for primary practices to use guidelines and identify the best available evidence if they can easily access all of the relevant guidelines from a single source, rather than each individual primary care practice trying to assemble all of the relevant guidelines itself. In some cases, such as diabetes, there are guidelines developed by different organizations that may differ in terms of the specific types of patients and situations they address, the most recent studies they used, and the interpretation of the results of those studies, and primary care physicians would likely find it helpful to know how to best utilize both sets of guidelines.
Guideline developers should work together to create a mechanism for primary care practices to easily access all of the guidelines that they would commonly use and to resolve any conflicts among different guidelines. For example, the American Medical Association could coordinate an effort by medical specialty societies and multi-stakeholder collaboratives to assemble the guidelines they have developed in a way that facilitates their use by primary care practices.
Keeping Clinical Practice Guidelines Up to Date
An enormous amount of time and effort is needed to assemble a set of clinical practice guidelines. In addition, every year, new medications and technologies are developed and there is new evidence about the appropriateness and effectiveness of different approaches to diagnosis and treatment, and so additional time and effort are needed to update guidelines so they incorporate the most current evidence and treatment options.
Government agencies (such as the Agency for Healthcare Research and Quality and the Centers for Medicare and Medicaid Services) and charitable foundations that want to improve the quality of healthcare should provide funding to medical specialty societies and multi-stakeholder collaboratives so they have the resources necessary to develop and maintain clinical practice guidelines free of commercial influence.
Creating Effective Clinical Decision Support
Good Clinical Practice Guidelines and Clinical Pathways are inherently detailed and complex because of the tremendous variation in the characteristics of patients and the characteristics of their health problems. This is also why they are better than the current approach to quality measurement, since most quality measures implicitly assume that the same approach to care is appropriate for all patients.
However, because clinical practice guidelines are complex, and because the diversity of patients seen by primary care physicians will require the use of multiple sets of guidelines, applying the appropriate guidelines to each patient will require a significant amount of time by the primary care physician and practice. This time is essential to high-quality care, and the amounts paid to the practice under Patient-Centered Primary Care Payment must be adequate to support this time.
The time required by a primary care practice to use Clinical Practice Guidelines or Pathways could potentially be reduced if the practice had access to an electronic Clinical Decision Support system that included all of the most current guidelines and that made it easy for the physician to identify and correctly apply the appropriate guideline or pathway.128 However, most current Clinical Decision Support systems or Electronic Health Records focus primarily on encouraging physician practices to adhere to narrowly-defined quality measures, rather than helping them identify and use the most appropriate evidence for each individual patient. The use of Patient-Centered Primary Care Payment could cause this to change, but the enhanced capability will likely also increase the amount the primary care practice will have to spend on an EHR system that has the appropriate capabilities.
The certification requirements for Electronic Health Record systems should be modified to require that the “clinical decision support” component of the EHR be based on all of the most current guidelines and that this component be easy for clinicians to use.
Physicians should not be required to use Clinical Decision Support systems, however. The “Meaningful Use” program created by the federal government demonstrated the problems of requiring physicians to use IT systems without first assuring that those systems work efficiently and effectively. Under Patient-Centered Primary Care Payment, physicians will have to use clinical practice guidelines, and if a CDS system works well at an affordable cost, physicians will likely want to use the CDS system. Vendors of such systems will then have a clear financial incentive to make sure they do work well for physicians and patients. However, the payments physicians receive for delivering services will need to be large enough to support the time and costs involved in buying and using CDS systems.
Supporting the Use of SCAMPs and Clinical Registries in Primary Care
Although existing Clinical Practice Guidelines for common conditions are extensive and detailed, they do not and cannot define what is best for every individual patient. In most cases, the evidence underlying the guidelines indicates which approaches to diagnosis and treatment have a higher probability of success for most patients, not which approach is best or is guaranteed to succeed for every patient. In particular, there is only limited evidence about which approaches are more effective for patients with multiple health problems or who face barriers in using standard approaches to diagnosis and treatment, so most guidelines provide less guidance about what to do in these cases.
This is why it is essential that the primary care physician have the flexibility to deviate from the guidelines when appropriate. The flexibility to deviate is particularly important when using Clinical Pathways. Pathways go beyond traditional Clinical Practice Guidelines by designating one preferred approach to diagnosis or treatment when evidence does not indicate which approach is clearly best. While clinical pathways can be desirable for reducing unnecessary variation in diagnosis and treatment, blindly following a pathway for every patient can result in some patients receiving inappropriate care. Many initiatives designed to improve care using clinical pathways expect that physicians will only do what is recommended in the pathway about 80% of the time, since there is not sufficient evidence to enable the pathway to define what is desirable for every individual patient. A significantly lower rate of adherence than this would suggest that there may be unnecessary variation in care, but a significantly higher rate of adherence could suggest that care is not being customized appropriately to patients’ needs. Significant deviations from any target adherence rate can only be used as an indicator that a more detailed examination of the reasons for deviation may be appropriate, not that services should automatically be viewed as inappropriate.
In addition, although detailed Clinical Practice Guidelines and Clinical Pathways are available for the most common conditions primary care physicians deal with, primary care physicians also see patients who have unusual problems for which there are no guidelines or where the guidelines are based on much more limited evidence. In these cases, primary care physicians must have the ability to use an approach to diagnosis and treatment that they and the patient believe will be best.
Moving From Guidelines/Pathways to SCAMPs
However, there must also be a process for developing the evidence necessary to fill the gaps in current clinical practice guidelines and to update the guidelines as new treatments and approaches to care delivery are developed. Although randomized control trials are the gold standard for generating evidence about whether a particular treatment is effective or more effective than other approaches, such trials are not feasible or appropriate in all cases, particularly when there are only small numbers of patients with specific characteristics and/or health problems.
As discussed in Section 4-C, a Standardized Clinical Assessment and Management Plan (SCAMP) is a mechanism for not only using existing evidence to guide decisions but also for filling the gaps in evidence where randomized trials are not feasible. Information collected about the situations in which deviations from the guidelines were needed or where the guidelines are silent can be analyzed by the physicians who are developing guidelines and pathways to assess the relative effectiveness of the approaches that are actually used for these patients in clinical practice. Findings from these analyses can then be used in an iterative fashion to provide preliminary guidance to primary care physicians about what approaches to use when similar cases appear in the future and to collect additional information on what is done and the outcomes that result. When sufficient evidence is available about what approaches are effective, it can be used to expand the formal guidelines.
Although SCAMPs for specialized services have been developed by small groups of interested physician practices and multi-physician specialty groups, SCAMPs for primary care will need a large number of physicians or practices to participate in order to generate enough information to provide an effective means of improving guidelines. An essential tool for collecting and analyzing data for a SCAMP from multiple physician practices is a Clinical Data Registry (CDR). A CDR is essentially a database that assembles information from multiple physician practices in a way that supports analysis and research on the effectiveness of different approaches to diagnosis and treatment for patients with specific characteristics.
A number of CDRs have been created by medical specialty societies and other groups that are being used for this purpose. For example, the American College of Cardiology’s PINNACLE registry was created in 2008 and has been used for more than a decade to analyze care processes and outcomes for patients with coronary artery disease, hypertension, heart failure, and atrial fibrillation.129 In 2014, the American College of Cardiology, the American College of Physicians, the American Diabetes Association, the American Association of Clinical Endocrinologists and the Joslin Diabetes Center created the Diabetes Collaborative Registry to play a similar role for patients with diabetes and prediabetes.130 The PINNACLE registry and the Diabetes Collaborative Registry are operated in a coordinated way, since many patients have both diabetes and heart conditions and one of the goals of effective treatment of diabetes is to prevent development or exacerbation of heart conditions.
Creating and maintaining registries is an expensive endeavor, both for the specialty societies that manage them and for the physician practices that submit data to them. Many existing registries have been forced to devote most of their time and resources to calculating narrowly-defined quality measures for pay-for-performance programs in order to make it worthwhile for physicians to participate, rather than expanding and strengthening the evidence for clinical practice guidelines. The Centers for Medicare and Medicaid Service has a program to designate “Qualified Clinical Data Registries” (QCDRs), but the requirements are focused on their ability to collect and report specific quality measures that CMS is willing to use in its Merit-Based Incentive Payment System (MIPS) program, not on trying to support the development of new evidence about what works and does not work effectively for patients who are not well served by typical quality measures.
Government agencies (such as the Agency for Healthcare Research and Quality and the Patient-Centered Outcomes Research Institute) and charitable foundations that want to support development of evidence about healthcare quality and effectiveness should provide funding to support the development of SCAMPs and the use of Clinical Data Registries.
Patient-Centered Primary Care Payment amounts should be large enough to ensure that primary care physicians have the resources needed to participate in CDRs and the time needed to document the reasons for deviations from guidelines in order to support a true SCAMP process.
Using a SAINT Designed for Primary Care
The use of Clinical Practice Guidelines/Pathways is necessary but not sufficient to ensure patients are receiving appropriate and high-quality care for health problems; the physician must also have a means to identify when their patients are having health problems and to determine whether prescribed treatments are working effectively for the patients. Similarly, documenting the reasons for deviations from existing guidelines is necessary but not sufficient for enabling a SCAMP to expand the evidence about what is effective; physicians must also have a way of collecting data on the outcomes that result from their treatment decisions.
This requires a Standardized Assessment, Information, and Networking Technology (SAINT). Fortunately, there is already a SAINT available for primary care called How’s Your Health that can be used immediately by primary care practices that participate in Patient-Centered Primary Care Payment.131 Although it is currently available for use at no cost to primary care practices thanks to the generosity of Dartmouth College and its faculty, it is unreasonable to expect that it can to continue to operate for free forever. Moreover, if additional resources were available, the capabilities of the system could be enhanced to make it easier for patients and physicians to use and to support its use as part of SCAMPs.
Government agencies (such as the Agency for Healthcare Research and Quality and the Patient-Centered Outcomes Research Institute) and charitable foundations that want to support development and use of patient-reported outcomes should provide funding to support enhancements to the How’s Your Health system. Patient-Centered Primary Care Payment amounts should be adequate to allow primary care practices to pay modest subscription fees to support the continued operation of How’s Your Health system and enhancements to its capabilities.
The use of How’s Your Health would not preclude the development or use of additional types of Patient Reported Outcome (PRO) measures. However, collecting and using such measures will require an investment of time and money by physician practices as well as by patients; those costs would need to be estimated and appropriate adjustments made in payments to the physician practices before the PROs could be used routinely.
Making Patient-Centered Primary Care Payment Available to Primary Care Practices
It does little good to define the CPT codes, appropriate RVU amounts, and adequate Conversion Factors necessary for implementation of Patient-Centered Primary Care Payment if health insurance plans, Medicare, and Medicaid programs are not willing to use them to pay primary care practices. Moreover, it will be difficult to justify doing the work needed to carry out these preparatory steps properly if there is little or no confidence that the work will actually be used by payers to improve the way primary care practices are paid.
A primary care practice would not be forced to wait for all of its current payers to implement Patient-Centered Primary Care Payment in order for the practice to deliver higher-quality care to at least a subset of its patients. Because primary care physicians will need to have smaller patient panels under Patient-Centered Primary Care Payment than they typically do today, a primary care practice could still receive sufficient revenues to cover its costs as long as a large-enough subset of its current payers implement the new payments. However, if one or more health plans refused to pay the practice using Patient-Centered Primary Care Payment, the practice would likely be forced to stop delivering care to the patients insured by those health plans, because it could not afford to do so with standard payments and it would be unfair to the patients whose plans are paying appropriately if the practice tried to deliver services to too many patients.
This is essentially what is happening today with primary care practices that convert to the Direct Primary Care model. Most Direct Primary Care practices don’t accept payments from any health insurance plans, and they have much smaller patient panels than other practices, which is one of the reasons primary care physicians have been attracted to this approach. When a primary care practice converts to Direct Primary Care, it has to tell its existing patients that it cannot continue providing care to them unless they are willing and able to pay the practice directly for their care (or if their employer will do so).
The goal should be to give every citizen the ability to receive high-quality primary care services regardless of what type of insurance they have, rather than exacerbate existing inequities in access to quality care. Consequently:
Every payer – every commercial insurance plan, every Medicare Advantage plan, every Medicaid Managed Care Organization, every state Medicaid agency, and Original (fee-for-service) Medicare – should make Patient-Centered Primary Care Payment available to any primary care practice providing services to the patients insured by that payer so that all patients have the opportunity to receive high-quality primary care.
Making Patient-Centered Primary Care Payment available to all primary care practices does not mean that a payer should require that every practice be paid in this way. Some practices may not be willing or able to immediately change the way they deliver care consistent with the expectations of Patient-Centered Primary Care Payment. There is no need to hold back the practices that are willing to change, or to delay payments for practices that are already delivering high-quality care and losing money doing so.
This is the same approach used in most existing Medicare and state multi-payer primary care payment programs. Participation by primary care practices is voluntary, so some primary care practices receive different payments while others continue to receive standard payments. Because Patient-Centered Primary Care Payment would use existing claims payment systems in response to billing codes submitted by the primary care practice, any payer could easily make the new payments to some primary care practices while continuing to pay other practices the same way they do today.
There is no need to mandate participation, because most primary care practices want a better system than they have today and most practices will likely want to participate once they see that a payer is implementing Patient-Centered Primary Care Payment properly. Moreover, once patients see how much better primary care can be under a better payment system, they will want to receive the kind of care that practices can deliver when they participate in the Patient-Centered Primary Care Payment system. As long as patients have a choice of which primary care practices to use, the patients can switch to a primary care practice that delivers patient-centered care, which will help to encourage practices to begin using Patient-Centered Primary Care Payment.
Ensuring that every payer makes Patient-Centered Primary Care Payment available to primary care practices will require different kinds of actions for each type of payer, including actions by citizens and businesses as well as health insurance companies and government insurance programs.
Changes in Payments From Private Insurance Plans
The majority of individuals living in the U.S. have health insurance from a commercial insurance plan, obtained either through their employer or directly from the insurance company. This is particularly true for individuals under age 65, who will receive some of the greatest long-term benefits of receiving good primary care. Consequently, it is essential that commercial insurance plans implement Patient-Centered Primary Care Payment.
Why Private Health Plans Are Unlikely to Change on Their Own
Unfortunately, it is unlikely that most private insurance companies will implement Patient-Centered Primary Care Payment without significant pressure from businesses and citizens. There are three reasons for this:
- Lower Profits from Higher Spending on Primary Care. For insurance plans funded through premiums, paying primary care practices more than they receive today will increase the insurance plan’s “medical loss” and reduce the insurance company’s profit. Even if higher-quality primary care results in an overall reduction in total health care spending, this is unlikely to occur immediately. Moreover, if a reduction in overall spending does occur, that would also cause a reduction in the health insurance plan’s profits. Under federal law, a commercial health insurance plan must spend 80-85% (i.e., the “minimum medical loss ratio”) of their premium revenues on healthcare services.132 That means that if there is a reduction in total healthcare spending, the insurance company would be required to reduce its administrative costs or profits.
- Administrative Costs for Implementation. Making changes in contracts with primary care practices, in benefit designs for patients, and in the internal systems used to make payments will temporarily increase the insurance company’s administrative costs, which will reduce its profits in the short term. The administrative cost of implementing Patient-Centered Primary Care Payment will be relatively small because the use of CPT codes will allow the payments to be implemented easily within the health insurance company’s existing claims payment system, and the additional costs will only occur temporarily when the changes are initially made. However, any increase at all in the plan’s administrative costs will translate into a reduction in profits for the insurance company. This is also true for insurance companies that are simply processing claims for self-insured businesses and other purchasers; even if the purchaser is willing to pay primary care practices differently, it needs a health insurance company or third-party administrator (TPA) that is willing to implement the changes in its claims processing system, and any increased administrative costs involved in that will reduce profits for the insurance company or TPA.
- Benefits From Being a Free Rider. In any community where there are multiple health plans, if most health plans implemented Patient-Centered Primary Care Payment, an individual plan would benefit by not doing so. A primary care practice will need to change the way it delivers services in order to succeed under Patient-Centered Primary Care Payment, and it will not want to deliver care to patients in different ways based on the type of insurance the patient has. Consequently, if a patient has insurance coverage from a “free rider” – a payer that does not implement Patient-Centered Primary Care Payment – the patient will likely receive the benefits of the higher-quality care while the patient’s insurance company avoids spending additional money on primary care services or incurring additional administrative costs. The free rider would make higher profits than the payers that do implement Patient-Centered Primary Care Payment, and the free rider could also charge lower premiums (or lower fees to self-insured businesses) in order to attract business away from the other health plans. Since every health plan would benefit from being a free rider, there is a disincentive for every health plan to implement the changes.
These problematic incentives also explain why the “primary care medical home payment” programs created by most health insurance plans fall far short of what primary care practices need. The two most common approaches are to provide small bonus payments based on claims-based quality measures or small monthly payments for each patient who is “attributed” to the primary care practice. These approaches are attractive because (a) the plan does not need to change its claims payment system at all, (b) the payments are very small so the impact on the plan’s spending is small, and (c) if the primary care practice actually improves care in a way that reduces reliance on office visits, the plan may save more from the reduction in spending on office visits than it pays in the bonuses or small monthly payments. However, these token changes do not actually solve the problems in the current payment system that prevent primary care practices from delivering higher-quality care or provide them with adequate revenues to do so.
Encouraging Health Insurance Plans to Use Patient-Centered Primary Care Payments
Most employers and citizens likely have no idea that the health insurance plan they are using is paying their primary care physician in a way that prevents the physician and primary care practice from delivering high-quality care. Even if they are aware of the problem, they may not know what they can do about it.
The strongest and perhaps only economic incentive for a health insurance plan to pay differently for primary care will be if it believes that doing so would significantly increase its membership or that failure to do so would cause it to lose a large number of customers. Consequently, it will be essential for employers and individuals to choose health insurance plans that pay primary care practices using Patient-Centered Primary Care Payment. No one employer or patient acting alone will have a big enough impact to change what health insurance companies do, particularly large insurance companies, so a large number of employers and individuals will all need to begin using health plans that implement Patient-Centered Primary Care Payment.
Self-insured purchasers should use health plans that implement Patient-Centered Primary Care Payment.
The decisions made by large employers about which health insurance plans to use will likely have the biggest impact on those plans’ willingness to change, simply because of the large number of plan members who will be affected.
The majority of individuals who have employer-sponsored health insurance in the U.S. are actually insured by their employer, not by the health insurance company that administers the plan. Most medium-size businesses do not buy health insurance policies for their employees per se, and hardly any large employers do. Instead, these employers are “self-insured,” meaning that they are at risk for spending on the covered healthcare services their employees receive, not the health insurance company. The health insurance company merely processes and pays the claims for services, and then sends a bill for the spending to the employer. This arrangement is referred to as “Administrative Services Only” (ASO) and the health insurance company is acting as a “Third Party Administrator” (TPA).
As a result, for self-insured employers, increases or decreases in spending on primary care affect the employer’s profits, not the profits of the health insurance company or TPA. Moreover, as discussed in Section 6-D, if primary care practices can deliver care more efficiently and effectively, the employer will benefit from improvements in employee productivity as well as any savings on other healthcare services. Conversely, there is no economic incentive for a health insurance company or TPA to pay primary care practices using Patient-Centered Primary Care Payment unless employers are choosing TPAs based on how they pay for primary care.
Consequently, if self-insured employers make it clear that they will only use TPAs that implement Patient-Centered Primary Care Payment, that will create a strong incentive for health insurance companies to implement them. Since a TPA is only processing claims and administering benefits, it does not need to be an insurance company, so if insurance companies are unwilling to implement Patient-Centered Primary Care Payment, other types of TPAs may be willing to do so.
Businesses should work together through purchaser coalitions to select health plans that implement Patient-Centered Primary Care Payment.
What matters to an individual primary care practice is how many of its own patients have insurance plans that pay for services using Patient-Centered Primary Care Payment. The majority of employers in any community are small businesses, and only a few patients in a primary care practice will be employees of the same employer, so if only one or two employers in the community change to a health plan that pays for services using Patient-Centered Primary Care Payment, that will have only a small impact on the practice’s revenues.
Moreover, because most of the businesses in a community are small, each of them will represent only a small proportion of a health insurance company’s business, so a decision by any one employer to change to a different health insurance plan will have little impact on health plans’ willingness to change the way they pay primary care practices. Even businesses that are large nationally because they have operations in many different communities typically employ only a small proportion of the total residents of any individual community.
However, by acting collectively, employers can have a much greater impact on what a health insurance company will be willing to do and on the revenues that primary care practices in the community will receive. The employers can accomplish this by forming a healthcare purchasing coalition and either using information assembled through the coalition to make similar decisions about which plans to purchase, or by having the coalition purchase health insurance or contract for TPA services collectively on their behalf. This is particularly important in regions where there is one dominant private health insurance company; other insurance companies are only likely to enter the market if there is a critical mass of purchasers that are willing to change the insurance plan they use.
A purchaser coalition does not need to be limited to one community or state. Since primary care practices in all communities want to be paid differently by private health plans, and since most health plans provide insurance in multiple communities and many provide insurance in multiple states, a bigger impact can be achieved if the employers in several communities work together collectively.
If a health plan is selling insurance to multiple employers in a region, it may also be more willing to sell insurance to individual community residents who purchase health insurance on an insurance exchange, so the actions employers in the community take could influence the individual insurance market as well as the group insurance market for their employees.
Purchasers should ensure that health plans implement Patient-Centered Primary Care Payment fully and correctly.
It will be important for employers and other purchasers to be precise about what it means for a health insurance plan to implement Patient-Centered Primary Care Payment for primary care practices. The same factors that lead health insurance plans to resist implementing Patient-Centered Primary Care Payment at all will give them an incentive to modify the structure of the payments in ways that are favorable to the plan but not necessarily favorable to primary care practices or their patients. For example, although the CMMI Comprehensive Primary Care Plus demonstration is represented as a multi-payer project, evaluations have shown that the payments made by commercial health plans that are nominally participating in the demonstration are smaller and structured differently from the payments Medicare is providing.133
Implementing Patient-Centered Primary Care Payment fully and correctly means both adding new payments in the right way and also taking away existing requirements:
- Payments Must Be Made for All of the New Billing Codes. The primary care practice should be paid for each of the new billing codes for patients who enroll for the services described in Section 4-B. Simply adding a new monthly payment on top of the existing structure does not solve the problems with the current payment system.
- The Payments for All New Billing Codes Must Be Adequate. The payment amounts for the new billing codes must be at the levels determined to be adequate through the process described in Section 4-D. It will do little good to change the method of payment if the amounts of payment are not adequate to allow the practice to spend adequate time with patients and hire the appropriate staff.
- Pay-for-Performance Programs Must Be Eliminated. The amounts the practice is paid should not be adjusted using quality or utilization measures, nor should the practice be financially penalized in any other way based on such measures. These programs simply increase administrative costs and take time away from patient care, and they do nothing to improve quality or reduce overall spending.
- Prior Authorization Requirements Must Be Eliminated. The practice should not be required to obtain prior authorizations for any of the services that it delivers or orders for patients. Prior authorization programs increase administrative costs and take time away from patient care, and they can harm patients.
- Patient Cost-Sharing Requirements Must Be Changed Appropriately. The payments should not be subject to deductibles, there should be no copayments or co-insurance for the monthly payments, and the cost-sharing for acute visits should be affordable for patients. It will do little good to improve the way primary care is delivered if patients cannot afford to receive it or are discouraged from doing so by unnecessary financial barriers.
It will be difficult for small employers and individuals to choose health insurance plans that use Patient-Centered Primary Care Payment if health plans do not provide clear information about the way they pay for primary care. Many health insurance plans tell businesses and patients that they are using “value-based payments” or “medical home payments” with no details on exactly what that means. To help address this:
- State insurance departments and state insurance exchanges could require health insurance plans to disclose the payment systems they use to pay primary care practices and to explicitly indicate whether Patient-Centered Primary Care Payment is one of the options available.
- Medical societies could survey primary care practices to find out which health plans have actually implemented Patient-Centered Primary Care Payment in the correct way.
If residents of the community have choices about which health insurance plan to use, primary care practices can refuse to contract with plans that do not use Patient-Centered Primary Care Payment.
Primary care practices can encourage health insurance companies to use Patient-Centered Primary Care Payment by refusing to contract with a health plan that does not. As long as there are health insurance plans that use Patient-Centered Primary Care Payment and that are affordable and available to residents of the community, the patients who want to continue receiving care from a high-quality practice could simply change to one of those health plans.134
Moreover, because health insurance plans are required to meet minimum standards for network adequacy, if a health insurance plan cannot contract with a sufficient number of primary care practices in a community, it will not be able to sell insurance in the community.
This strategy will work best if the primary care practices in the community work collaboratively with employers or a purchasing coalition in a coordinated effort to change the way all health insurance plans pay for primary care services:
- In order for employers to switch health plans based on the method the plan uses to pay for primary care, they will want to know there are primary care practices that will deliver better care to their employees using those payments.
- If most of the employers in the community are moving toward health plans that use Patient-Centered Primary Care Payment, it will be more likely that all of a practice’s patients will have such plans available to them and the practice can implement the necessary changes in care delivery.
In a number of communities, non-profit multi-stakeholder Regional Health Improvement Collaboratives have brought multiple payers and providers together to agree on a common payment methodology to support improved care delivery.135 Although concerns are often raised about whether such discussions violate antitrust law, antitrust prohibitions focus primarily on payers or providers agreeing on a common price for services, not on developing a common method of payment.136 An alternative approach is for state governments to coordinate statewide or community-wide implementation of Patient-Centered Primary Care Payment, using the state action exemption under federal antitrust law.
Changes in Medicare Payments
The second largest group of patients is Medicare beneficiaries. In order to deliver high-quality primary care to all Medicare beneficiaries, primary care practices need to receive Patient-Centered Primary Care Payment from both Original Medicare and Medicare Advantage plans.
Changing the Way Medicare Advantage Plans Pay for Primary Care
More than one-third of Medicare beneficiaries are enrolled in Medicare Advantage (MA) plans. These plans receive a capitated payment from CMS for each beneficiary who enrolls in the plan. Each Medicare Advantage plan is required to pay for the same kinds of services that are covered under Original Medicare, but the plan is not required to pay healthcare providers the same amounts or the same way as Original Medicare pays or to use the same cost-sharing formulas for beneficiaries.
Unfortunately, since they are private health insurance plans, Medicare Advantage plans are likely to resist implementing Patient-Centered Primary Care Payment for all of the same reasons described earlier for other private insurance plans, i.e., the impacts on their administrative costs and profits and the advantages of being a free rider. Similarly, the only significant economic incentive for a Medicare Advantage plan to change the way it pays primary care practices will be if it believes that it would increase its membership by doing so or that failure to do so will cause it to lose members.
Two approaches will help create the necessary incentives for Medicare Advantage plans to implement Patient-Centered Primary Care Payment:
Medicare beneficiaries who have chosen to enroll in a Medicare Advantage plan should choose a plan that makes Patient-Centered Primary Care Payment available to primary care practices.
Most Medicare beneficiaries likely have no idea that the Medicare Advantage plan they choose because of low premiums and other benefits may be helping to force their primary care practice out of business, or that their primary care physician could provide them with better care if their health insurance plan paid in a different way.
In 2021, the average Medicare beneficiary could choose among 33 Medicare Advantage plans, but more than half did not even compare the options.137 In order for beneficiaries to select plans that use Patient-Centered Primary Care Payment, they could simply ask their primary care physician which MA plans pay that way. Alternatively, either CMS or state insurance departments could require MA plans to disclose the payment systems they use to pay primary care practices and to explicitly indicate whether Patient-Centered Primary Care Payment is one of the options available, so the information can be provided to Medicare beneficiaries.
If Original Medicare implements Patient-Centered Primary Care Payment, Medicare beneficiaries could also choose to remain in Original Medicare or switch back to Original Medicare rather than enrolling in a Medicare Advantage plan.
Primary care practices can refuse to contract with Medicare Advantage plans that do not use Patient-Centered Primary Care Payment.
Primary care practices can encourage Medicare Advantage plans to use Patient-Centered Primary Care Payment by refusing to contract with those that do not. Since most Medicare beneficiaries have a choice of Medicare Advantage plans as well as the choice of remaining in Original Medicare, even if a beneficiary’s primary care practice stops contracting with the beneficiary’s current insurance plan, the beneficiary could continue to receive care from the practice simply by changing plans.
Moreover, if a Medicare Advantage enrollee receives care from a provider that is not contracting with the patient’s MA plan, the plan is required to pay the provider the same amounts that would be paid under Original Medicare. If Patient-Centered Primary Care Payment is implemented for Original Medicare beneficiaries, the practice could still deliver care to the beneficiary and be paid adequately and appropriately. Since Medicare Advantage plans are required to meet minimum standards for network adequacy, if a plan does not contract with a sufficient number of primary care practices in a community, it will not be able to continue enrolling Medicare beneficiaries in the community.
Changing the Way Original Medicare Pays for Primary Care
The Wrong Way: Changing Payments Through CMMI Demonstrations
Over the past decade, many primary care practices have been able to receive significantly higher and more flexible payments for services delivered to Original Medicare beneficiaries by participating in primary care demonstration projects created by the Center for Medicare and Medicaid Innovation (CMMI). The primary care practices that are participating in the Comprehensive Primary Care Plus (CPC+) initiative, particularly those in Track 2 of CPC+, have much greater flexibility in delivering services to Medicare beneficiaries and they receive significantly more revenues for doing so than through standard Medicare payments or through the primary care payment programs available from commercial health plans and Medicare Advantage Plans.
Unfortunately, as discussed in Section 5-D, the “hybrid” payment structure used in CPC+ fails to fully solve the problems in the current payment system. However, rather than building on the positive features in CPC+ and correcting its weaknesses, CMMI is terminating CPC+ at the end of 2021 and replacing it with a much more problematic payment system called Primary Care First.
In addition to the problems with the payment systems CMMI has designed in these programs, there are also serious problems with the approach CMMI uses in implementing primary care payment changes:
- Only a subset of primary care practices can participate. Because of the need to conduct a formal evaluation of any payment changes and to have a control group that is not being paid in that way, only primary care practices located in selected states and regions have been able to participate in the CMMI primary care demonstrations, and even in those states/regions, only a subset of primary care practices are permitted to participate. As a result, most primary care practices in the country are only able to be paid for services to Original Medicare beneficiaries with standard fee-for-service payments.
- Temporary rather than permanent changes in payments. The payment changes that are made available through CMMI are only temporary, and they are scheduled to end after at most five years. By statute, CMMI is limited to “testing models,” and it cannot continue a change in payment unless an evaluation shows that it meets the statutory criteria for doing so. However, most primary care practices are not going to be willing to make significant changes in the way they deliver care that are dependent on receiving the new payments if they believe the payments will end after a few years. Consequently, the impacts on quality and spending will likely be less than what could be achieved if primary care practices knew that they could count on receiving the payments in the long term.
- Unrealistic standards for continuation of payments. Congress required CMMI to focus on projects that would reduce Medicare spending, and it is prohibited from continuing a demonstration unless an evaluation shows that net spending will not increase.138 No matter how much the demonstration improves the quality of care, if Medicare net spending increases, the demonstration is terminated. The first CMMI primary care demonstration (the Comprehensive Primary Care Initiative) was terminated because it did not reduce Medicare spending. It was replaced by CPC+, which is also now being terminated because it has not been found to reduce Medicare spending.139
As discussed in Section 6, the goal of primary care should be to improve health, not to reduce healthcare spending, and it is unrealistic to expect that adequate payments for primary care will result in a net reduction in total spending, particularly during the 5-year time period typically used to evaluate CMMI demonstration projects. As a result, it is unlikely that any primary care payment reform program implemented by CMMI will ever be made permanent, regardless of how it is structured. There is little reason to continue conducting demonstration projects in primary care if the goal (reducing net spending) is impossible to achieve, particularly during any short-term demonstration.
Moreover, because of the requirement to reduce spending rather than to support and sustain high-quality primary care services, it is unlikely that CMMI would ever implement Patient-Centered Primary Care Payment. As explained in Section 5-D, CMMI’s new Primary Care First program pays primary care practices less than they would receive under either CPC+ or Patient-Centered Primary Care Payment, and it inappropriately places a large portion of their payments at risk based on performance on utilization and quality measures they cannot control. As discussed in Section 5-E, CMMI has also created a separate program called Direct Contracting that would require a primary care practice to be at financial risk for Medicare spending on all of the services their patients receive from specialists and hospitals. By failing to address the problems in the current payment system and placing unrealistic financial risk on primary care practices, these programs are more likely to accelerate the loss of primary care providers than to achieve greater savings for Medicare. Moreover, if CMMI convinces other payers to participate in its models, that would give those payers another reason not to implement Patient-Centered Primary Care Payment.
Because of all of these constraints and problems, the Center for Medicare and Medicaid Innovation (CMMI) is not and cannot be the appropriate mechanism for improving the way primary care practices are paid in Medicare.
The Right Way: Changing the Medicare Physician Fee Schedule
The only way to ensure that every Medicare beneficiary can receive high-quality primary care is to enable every primary care practice to receive Patient-Centered Primary Care Payment for their patients who have Original Medicare insurance. The only way to do this is to add the billing codes for Patient-Centered Primary Care Payment to the Medicare Physician Fee Schedule.
CMS has the statutory authority to add the new billing codes for Patient-Centered Primary Care Payment to its fee schedule and to allow every primary care practice in the country to bill for them. In fact, over the course of several years, it created a number of new fees to support enhanced services delivered by primary care practices. For example, Medicare now pays fees for delivery of chronic condition management services to certain kinds of patients, it pays fees for collaborative behavioral health care, and it pays fees for transitional care services to patients who have been discharged from the hospital; each of these payments has helped fill some of the gaps in fee-for-service payment. In 2020, CMS dramatically increased the flexibility of primary care practices (and also specialty care practices) to provide services to patients in different and better ways by paying for services when they were delivered by telehealth to patients in their home and paying for evaluation and management services when they were delivered by telephone.
Just as there is no requirement that primary care practices use any of the new billing codes that Medicare has already created, there does not need to be any requirement that primary care practices use the billing codes created for Patient-Centered Primary Care Payment for Medicare beneficiaries. However, if a primary care practice billed for services to a patient using one of the new Patient-Centered Primary Care Payment codes, it would not bill or be paid using existing billing codes for evaluation and management services during the same month, as discussed in Section 7-A. Like every other payer, Medicare has payment systems with the ability to ensure that a practice is not paid for both sets of codes for the same patient in the same month.
Enabling Adequate Payment Amounts in Medicare and Exempting Patient-Centered Primary Care Payment from Budget Neutrality Requirements
Although CMS has the statutory authority to add the new billing codes for Patient-Centered Primary Care Payment to its fee schedule, it likely does not have the necessary authority to pay adequate amounts for those billing codes. As discussed in Section 7-A, current payments for primary care practices are inadequate because the Conversion Factor used in Medicare is too low. The Update Factors that Congress requires CMS to use have been below the rate of inflation for many years, and since the Update Factor will be zero in the future, payments will become even more inadequate in the future. Congressional action will be needed to address this.
In addition, as discussed in Section 7-A, statutory budget neutrality rules require that any significant increase in payments to primary care practices be accompanied by a corresponding reduction in the Conversion Factor in order to avoid a significant overall increase in spending on physician services. Primary care practices will be able to use the Patient-Centered Primary Care Payment codes for more patients than are eligible for some of the current billing codes (e.g., a practice could bill for Chronic Condition Management payments for all patients with a chronic disease, rather than only the subset of patients with two or more chronic diseases who are eligible for current Chronic Care Management billing codes) and the new codes will be specifically designed so that physicians and other practice staff can spend more time with patients. Consequently, when primary care practices use the new codes, Medicare spending on primary care will increase, and that would force reductions in payments for all other services. It doesn’t matter whether improved primary care helps patients avoid hospitalizations, because the law does not allow CMS to consider savings in hospital spending as offsets for higher payments to primary care physicians. Congressional action will be needed to solve this problem.
Congress should create a Patient-Centered Primary Care Payment program for Original Medicare beneficiaries with the following characteristics:
- All primary care practice should be able to voluntarily enroll, and no primary care practice should be forced to participate;
- CMS should implement all of the new billing codes for Patient-Centered Primary Care Payment in the Medicare Physician Fee Schedule and assign payment amounts to the codes that are adequate to support high-quality primary care services;
- The program should exempt participating primary care practices from the current Merit-Based Incentive Payment System (MIPS) and base accountability for quality and utilization on the utilization of clinical practice guidelines and SCAMPs;
- Any net increase in spending on primary care should be exempt from budget neutrality calculations.
Congress has authorized higher payments for primary care practices in the past; for example, the Affordable Care Act required a 10% increase in payments for several years. However, the increases that will be needed to ensure adequate payments for primary care will be much larger than this. Because primary care is only a small portion of total spending, large increases in spending on primary care do not have a large impact on total Medicare spending. As discussed in Section 6-B, doubling Medicare payments for primary care would only increase total Medicare spending by about 5%, and if higher-quality primary care reduces spending on other types of services, the net increase in Medicare spending would be even less.
Creating a permanent, voluntary program for Patient-Centered Primary Care Payment would be similar to what Congress did when it created the Medicare Shared Savings Program – it is a permanent part of the regular Medicare program, not a temporary demonstration project created by CMMI; participation by physicians is voluntary, not mandatory; and participants in the program are eligible for additional payments that are not available to non-participants, while still being able to bill for and be paid the standard amounts for other services.
Changes in Medicaid Payments
Finally, state Medicaid programs need to implement Patient-Centered Primary Care Payment so that Medicaid beneficiaries can receive the benefits of better primary care. Failure to do so would exacerbate existing inequities in access to high-quality healthcare services for individuals under age 65 who are unable to work and for individuals and families with low incomes.
However, two different approaches will be needed because states use two different mechanisms for providing benefits to Medicaid beneficiaries:
- In most states, primary care practices and other healthcare providers are now paid by Medicaid Managed Care Organizations (MCOs) rather than directly by the state. Medicaid MCOs are typically health insurance companies that the state Medicaid agency has contracted with to “manage” healthcare services for most or all Medicaid beneficiaries. The MCO receives a capitated payment from the state for each Medicaid beneficiary, and the MCO then pays healthcare providers for all of the services they deliver to the beneficiary, typically using fees for individual services.
- In some states, however, the state Medicaid agency still directly pays healthcare providers for services they deliver to eligible individuals.
Changing Payments in States With Medicaid MCOs
Medicaid MCOs will be unlikely to implement Patient-Centered Primary Care Payment voluntarily for the same reasons described earlier for commercial insurance plans and Medicare Advantage plans. Paying primary care practices more and changing the method used to pay them will reduce the MCOs’ profits in the short run, and each MCO can benefit by being a free rider.
If MCOs begin spending more on primary care, the state Medicaid agency will have to pay the MCOs more, since federal law requires that the MCO receive an “actuarily sound” payment from the state.140 However, in the longer run, the actuarily sound payments might increase even more if payments for primary care are not increased, since poor access to primary care could cause Medicaid beneficiaries’ health to worsen, resulting in a greater need for more expensive healthcare services. This means that failure to increase payments for primary care practices could result in the highest profits for MCOs both in the short run and long run.
State Medicaid programs cannot simply require MCOs to change the way they pay primary care practices, because regulations issued by the Centers for Medicare and Medicaid Services (CMS) limit states’ ability to specify how MCOs should pay healthcare providers or how much they should pay. Under the regulations, a state is only permitted to require that a Medicaid MCO implement a “value-based purchasing model” that is “intended to recognize value or outcomes over volume of services” or to require an MCO to participate in a “delivery system reform or performance improvement initiative.” Moreover, CMS requires that any payments the MCO is required to make must be “based on the utilization and delivery of services” and “advance at least one of the goals and objectives in the state’s quality strategy.” If a state wants to require such a payment model, it has to receive approval from CMS before it can do so, and the arrangement “cannot be renewed automatically.”141
It will be very slow and inefficient if every state is forced to submit a separate request to CMS to require Medicaid MCOs to implement Patient-Centered Primary Care Payment, wait for CMS to review the request, make revisions in response to CMS questions, and then wait for final approval. In order for primary care practices to get adequate and appropriate Medicaid payments as quickly as possible, both the federal and state governments need to take action.
CMS should establish a policy indicating that approval will automatically be given to states that want to require Medicaid Managed Care Organizations (MCOs) to use Patient-Centered Primary Care Payment.
The design of the Patient-Centered Primary Care Payment system clearly satisfies the requirements for a “value-based purchasing model” or “delivery system reform initiative” under CMS regulations. Because primary care practices would still receive fees for individual services under a Patient-Centered Primary Care Payment system, it meets the requirement that payments be based on the utilization and delivery of services. Because the payments are only made if services meet quality standards, Patient-Centered Primary Care Payment satisfies CMS requirements that payments advance quality goals and recognize value over volume. If CMS does not believe that Patient-Centered Primary Care Payment meets those regulatory requirements, it should change the regulations, rather than force undesirable changes that could harm primary care practices.
In states that use Medicaid MCOs, the state Medicaid agency should require MCOs to use Patient-Centered Primary Care Payment to pay primary care practices that wish to participate.
The state Medicaid agency should work with the state’s primary care practices to ensure that MCOs are implementing the payments correctly. If purchaser coalitions in the state are working to encourage implementation of Patient-Centered Primary Care Payment by private health plans, it would be desirable for the state to also participate as a purchaser in order to ensure a coordinated, multi-payer approach, since a number of commercial health insurance companies also serve as Medicaid MCOs.
Changing Payments in States That Do Not Use Medicaid MCOs
Things are simpler in states that do not use Medicaid MCOs, since they can directly decide how healthcare providers should be paid for their services.
In states that do not use Medicaid MCOs, the state Medicaid agency should begin using Patient-Centered Primary Care Payment to pay primary care practices that wish to participate.
Funding to Ensure Adequate Payments for Primary Care in Medicaid
In most states, Medicaid payments for primary care services are well below Medicare payment levels. In 2019, average Medicaid payments for primary care were only 67% of Medicare payment amounts, and in several states, Medicaid payments were less than half of Medicare amounts.142
As a result, in most states, Medicaid spending on primary care will have to more than double in order to provide adequate payments for primary care services to individuals on Medicaid. Since current spending on primary care represents only about 6% of total Medicaid spending143, doubling or tripling the amount spent on primary care could require about a 6-12% increase in total Medicaid spending. The magnitude of the increase would vary from state to state depending on how much is currently being spent both on primary care and how much is spent on other services.144
As discussed in Section 6-C, providing better access to higher-quality primary care will likely result in savings on other services, so the net increase in spending will be lower than this. However, it is unreasonable to expect that there will enough savings to offset all of the higher spending on primary care, particularly in the short run, so state legislatures will have to budget more for Medicaid in order to ensure payments for primary care are adequate.
Congress could encourage and assist states in making this investment by paying for a portion of the increased spending. For example, in addition to increasing Medicare payments for primary care, the Affordable Care Act increased Medicaid primary care physician fees to Medicare levels in 2013 and 2014, and 19 states continued all or part of the higher payment rates at least in the first year after that increase expired.145
Summary of Implementation Actions
ACTIONS NEEDED TO IMPLEMENT
PATIENT-CENTERED PRIMARY CARE PAYMENT
Operationalizing Billing and Payment
- The CPT Editorial Panel should establish a formal definition for each of the patient-centered primary care services and assign a specific CPT code to that definition.
- The RVS Update Committee (RUC) should assign appropriate RVU amounts for each of the new CPT codes for the Patient-Centered Primary Care Payments.
- Medicare and health insurance plans should use appropriate Conversion Factors to convert the RVUs into adequate payments for participating primary care practices. Analyses should be carried out by the RUC or an organization such as the Patient-Centered Primary Care Collaborative or the Medical Group Management Association in order to determine an appropriate conversion factor for Patient-Centered Primary Care Payment CPT codes.
Operationalizing Accountability for Quality and Utilization
- Government agencies and charitable foundations should provide funding to medical specialty societies and multi-stakeholder collaboratives to support development and maintenance of clinical practice guidelines that are free of commercial influence.
- Guideline developers should work together to create a mechanism for enabling primary care practices to easily access all of the guidelines that they would commonly use and to resolve any conflicts among different guidelines.
- The certification requirements for Electronic Health Record systems should be modified to require that the “clinical decision support” component of the EHR be based on all of the most current guidelines and that this component be easy for clinicians to use.
- Government agencies and charitable foundations should provide funding to support the development of SCAMPs and the use of Clinical Data Registries (CDRs).
- Patient-Centered Primary Care Payment amounts should be large enough to ensure that primary care physicians have the resources needed to participate in CDRs and the time needed to document the reasons for deviations from guidelines.
- Government agencies and charitable foundations should provide funding to support enhancements to the How’s Your Health system.
- Patient-Centered Primary Care Payment amounts should be adequate to allow primary care practices to pay modest subscription fees to support the continued operation of the How’s Your Health system.
Making Patient-Centered Primary Care Payment Available to Primary Care Practices
Every payer – every commercial insurance plan, every Medicare Advantage plan, every Medicaid Managed Care Organization, every state Medicaid agency, and Original (fee-for-service) Medicare – should make Patient-Centered Primary Care Payment available to any primary care practice providing services to the patients insured by that payer so that all patients have the opportunity to receive high-quality primary care. However, primary care practices should not be required to participate if they do not wish to.
Changes in Payments From Private Insurance Plans
- Self-insured purchasers should use health plans that implement Patient-Centered Primary Care Payment.
- Businesses should work together through purchaser coalitions to select health plans using Patient-Centered Primary Care Payment.
- Purchasers should ensure that health plans implement Patient-Centered Primary Care Payment fully and correctly. This means:
- Payments must be made for all of the new billing codes.
- The payments for all new billing codes must be adequate.
- Pay-for-performance programs must be eliminated.
- Prior authorization requirements must be eliminated.
- Patient cost-sharing requirements must be changed appropriately.
- If residents of the community have choices about which health insurance plan to use, primary care practices can refuse to contract with plans that do not use Patient-Centered Primary Care Payment.
Changes in Medicare Payments
- Congress should create a Patient-Centered Primary Care Payment program for Original Medicare beneficiaries structured as follows:
- All primary care practices should be able to voluntarily enroll, but no primary care practice should be forced to participate;
- CMS should implement all of the new billing codes for Patient-Centered Primary Care Payment and assign payment amounts to the codes that are adequate to support high-quality primary care services.
- The program should exempt participating primary care practices from the current Merit-Based Incentive Payment System (MIPS), and instead should base accountability for quality and utilization on the utilization of clinical practice guidelines and SCAMPs.
- Any net increase in spending on primary care should be exempt from budget neutrality calculations.
- Medicare beneficiaries who have chosen to enroll in a Medicare Advantage plan should choose a plan that makes Patient-Centered Primary Care Payment available to primary care practices. In addition, primary care practices can refuse to contract with Medicare Advantage plans that do not use Patient-Centered Primary Care Payment.
Changes in Medicaid Payments
- CMS should establish a policy indicating that approval will automatically be given to states that want to require Medicaid Managed Care Organizations (MCOs) to use Patient-Centered Primary Care Payment.
- In states that use Medicaid MCOs, the state Medicaid agency should require MCOs to use Patient-Centered Primary Care Payment for primary care practices that wish to participate.
- In states that do not use Medicaid MCOs, the state Medicaid agency should begin using Patient-Centered Primary Care Payment to pay primary care practices that wish to participate.
Accelerating Payment Reform for Primary Care
Although there has been widespread consensus for many years about the need to improve the way primary care practices are paid, no meaningful reforms have occurred. As a result, there is a large and growing shortage of primary care physicians in the country146, many primary care physicians are burning out147, and most medical students don’t want to go into primary care.148
It is time to stop making small changes to current payment systems and expecting significant results. It is time to stop imposing reporting and accreditation requirements that do nothing to improve outcomes for patients while discouraging physicians from practicing primary care. It is time to stop creating small-scale demonstration programs with inadequate resources and unrealistic goals for reducing spending and improving outcomes, then waiting for years until evaluations are completed before considering better approaches. It is time to stop believing that health insurance plans will design and implement appropriate primary care payment reforms when they have no financial incentive to do so. These approaches have been used for over a decade and they have failed to address the serious problems facing primary care. There is no reason to believe that any better results will be achieved by continuing on the same path.
Payments for primary care will not be better simply because they are different from the current fee-for-service system. It is clear that current and commonly proposed approaches to primary care payment reform have serious flaws that fail to improve the quality of care, fail to reverse the loss of primary care physicians, and can harm vulnerable patients.
Patient-Centered Primary Care Payment will address the problems in the current primary care payment system and provide primary care practices with the support they need to deliver high quality care for all patients, including those with complex needs. Although the details of this payment system will likely need to be adjusted to ensure it works effectively for all practices and all types of patients, these adjustments can and should be made over time after the payment system is operational. Conversely, it will be impossible to determine what payment amounts or service definitions are exactly right until primary care practices are actually able to deliver care differently. Delaying implementation of a patient-centered payment system until consensus is reached on the ideal approach to every detail will prevent patients from receiving the better-quality care they need right now, and it will likely result in additional losses of primary care practices in the interim. Moreover, the question should not be whether businesses and government agencies can afford to pay primary care practices adequate amounts, but whether they can afford not to.
The leadership for true reform will need to come from primary care physicians, employers, and citizens. They are directly affected by the problems in the current payment system, and they will receive the benefits in terms of better health and higher productivity, not health insurance plans. The future of primary care will depend on whether purchasers, patients, and primary care practices work together to take the actions necessary to implement a truly patient-centered primary care payment system.
Footnotes
Starfield B, Shi L, Macinko J. “Contribution of Primary Care to Health Systems and Health.” The Milbank Quarterly 83(3):457-502 (2005).↩︎
Binns HJ et al. “Describing Primary Care Encounters: The Primary Care Network Survey and the National Ambulatory Medical Care Survey.” Annals of Family Medicine 5(1):39-47 (2007).↩︎
Miller HD. Why Value-Based Payment Isn’t Working, and How to Fix It. Center for Healthcare Quality and Payment Reform (2017).↩︎
For example, the use of corticosteroids in treating patients with severe asthma or COPD can increase blood sugar levels and make it more difficult to treat diabetes if the patient is also diabetic.↩︎
Wolk CB et al. “Improving Payment for Collaborative Mental Health Care in Primary Care.” Medical Care 59(4):324-326 (2021).↩︎
American Psychiatric Association and Academy of Psychosomatic Medicine. Dissemination of Integrated Care Within Adult Primary Care Settings: The Collaborative Care Model (2016).↩︎
American Psychological Association. Behavioral Health Services in Primary Care.↩︎
This is similar to the process currently used in Medicare for its Chronic Condition Management (CCM) payments. In order for a physician to receive CCM payments for a particular patient, they must obtain consent from that patient. Consent may be verbal or written but must be documented in the medical record. Centers for Medicare and Medicaid Services. Chronic Care Management Services. CMS Medicare Learning Network MLN909188 (July 2019).↩︎
For example, the International Consortium for Health Outcomes Measurement (ICHOM) Older Persons Working Group recommended that healthcare providers and payers use thirteen different measures of outcomes for older people. Two of the most important measures (“place of death,” “frailty”) would be of little relevance to younger populations. Akpan A et al. “Standard Set of Health Outcome Measures for Older Persons.” BMC Geriatrics 18:36 (2018).↩︎
Nano J et al. “A Standard Set of Person-Centred Outcomes for Diabetes Mellitus: Results of an International and Unified Approach.” Diabetic Medicine 37:2009-2018 (2020)↩︎
Nano J et al. op. cit.↩︎
Tseng C et al. “Association of Serious Hypoglycemic Events in Older Adults With Changes in Glycemic Performance Measures.” Medical Care (2021). Rodriguez-Gutierrez R, McCoy RG. “Measuring What Matters in Diabetes.” JAMA 321(19): 1865-1866 (2019).↩︎
Cramer JA. “A Systematic Review of Adherence With Medications for Diabetes.” Diabetes Care 27(5):1218-1224 (2004).↩︎
Mendelson A, Kondo K, Damberg C et al. “The Effects of Pay-for-Performance Programs on Health, Health Care Use, and Processes of Care – A Systematic Review.” Annals of Internal Medicine 166(5):341-353 (March 2017).↩︎
Casalino LP et al. “U.S. Physician Practices Spend More Than $15.4 Billion Annually to Report Quality Measures,” Health Affairs 35(3): 401-406 (2016).↩︎
MacLean CH, Kerr EA, Qaseem A. “Time Out - Charting a Path for Improving Performance Measurement.” The New England Journal of Medicine 378:1757-1761 (2018).↩︎
Vijan S et al. “Effects of Patients’ Risks and Preferences on Health Gains With Plasma Glucose Level Lowering in Type 2 Diabetes Mellitus.” JAMA Internal Medicine 174(8):1227-1234 (2014).↩︎
Resneck JS. “Refocusing Medication Prior Authorization on Its Intended Purpose.” JAMA 323(8):703-704 (2020).↩︎
Casalino LP et al. “What Does It Cost Physician Practices to Interact With Health Insurance Plans?” Health Affairs 28(4):w533-w543 (2009).↩︎
Sox HC, Stewart WF. “Algorithms, Clinical Practice Guidelines, and Standardized Clinical Assessment and Management Plans: Evidence-Based Patient Management Standards in Evolution.” Academic Medicine 90(2) (2015).↩︎
Kuntz G. “What Do We Mean When We Talk About ‘Clinical Pathways?’” Journal of Clinical Pathways January/February 2019.↩︎
Rotter T et al. “Clinical Pathways: Effects on Professional Practice, Patient Outcomes, Length of Stay and Hospital Costs.” Cochrane Database of Systematic Reviews CD006632 (2010).↩︎
Toy JM, Drechsler A, Waters RC. “Clinical Pathways for Primary Care: Current Use, Interest and Perceived Usability.” Journal of the American Medical Informatics Association 25(7):901-906 (2018).↩︎
Carlsen B, Glenton C, Pope C. “Thou Shalt Versus Thou Shalt Not: A Meta-Synthesis of GPs’ Attitudes To Clinical Practice Guidelines.” British Journal of General Practice 57:971-978 (2007).↩︎
Spencer-Bonilla G, Quiñones AR, Montori VM. “Assessing the Burden of Treatment.” Journal of General Internal Medicine 32(10):1141-1145 (2017).↩︎
Grimso A et al. “Disease-Specific Clinical Pathways – Are They Feasible in Primary Care? A Mixed-Methods Study.” Scandinavian Journal of Primary Health Care 36(2):152-160 (2018).↩︎
Farias M et al. “Standardized Clinical Assessment and Management Plans (SCAMPs) Provide A Better Alternative to Clinical Practice Guidelines.” Health Affairs 32(5):911-920 (2013).↩︎
Kuhlman J et al. “Clinical Transformation Through Change Management Case Study: Chest Pain in the Emergency Department.” EClinical Medicine 10 (2019).↩︎
Farias M et al. “Provider Attitudes Toward Standardized Clinical Assessment and Management Plans (SCAMPs).” Congenital Heart Disease 6(6):538-565 (2011).↩︎
Wasson JH. “Standardized Assessment, Information, and Networking Technologies (SAINTs): Lessons From Three Decades of Development and Testing.” Quality of Life Research (2020).↩︎
Ibid.↩︎
Ho L, Antonucci J. “Using Patient-Entered Data to Supercharge Self-Management” Annals of Family Medicine 15(4):382 (2017).↩︎
Wasson JH et al. “Development of a Care Guidance Index Based on What Matters to Patients.” Quality of Life Research 27:51-58 (2018).↩︎
Wasson JH, Ho L, Soloway L, Moore LG. “Validation of the What Matters Index: A brief, patient-reported index that guides care for chronic conditions and can substitute for computer-generated risk models.” PLoS ONE 13(2): e0192475.↩︎
Wasson JH et al. “Patients Use the Internet to Enter the Medical Home.” Journal of Ambulatory Care Management 34(1):38-46 (2011).↩︎
Hughes C. “Medicare Annual Wellness Visits: Don’t Forget The Health Risk Assessment.” Family Practice Management March/April 2012, pp. 11-14.↩︎
Ho L et al. “The Right Tool for the Right Job: The Value of Alternative Patient Experience Measures.” Journal of Ambulatory Care Management 36(3):241-244 (2013).↩︎
Kupfer JM, Bond EU. “Patient Satisfaction and Patient-Centered Care: Necessary But Not Equal.” JAMA 308(2):139-140 (2012).↩︎
Hart CWL. “The Power of Unconditional Service Guarantees.” Harvard Business Review July-August 1988, pp 54-62; Kandampully J, Butler L. “Service Guarantees: A Strategic Mechanism to Minimise Customers’ Perceived Risk in Service Organizations.” Managing Service Quality 11(2):112-120 (2001); Fruchter GE, Gerstner E. “Selling With ‘Satisfaction Guaranteed.’” Journal of Service Research 1(4): 313-323 (1999); Lutz NA. “Warranties as Signals Under Consumer Moral Hazard,” RAND Journal of Economics 20(2): 239-255 (1989).↩︎
Doran T et al. “Exclusion of Patients from Pay-for-Performance Targets by English Physicians.” The New England Journal of Medicine 359(3):274-284 (2008).↩︎
Persell SD et al. “Frequency of Inappropriate Medical Exceptions to Quality Measures.” Annals of Internal Medicine 152(4):225-231 (2010).↩︎
Doran T et al. “Exempting Dissenting Patients from Pay for Performance Schemes: Retrospective Analysis of Exception Reporting in the UK Quality and Outcomes Framework.” BMJ 344:e2405 (2012)↩︎
Medicare rules for physician office visits state that “the provider must ensure that the submitted claim accurately reflects the services provided. The provider must also ensure that medical record documentation supports the level of service reported to a payer.” Centers for Medicare and Medicaid Services. Evaluation and Management Services Guide. CMS Medicare Learning Network Booklet MLN906764 (February 2021).↩︎
The Medical Group Management Association reports benchmarking data for physician practices in terms of costs per full-time-equivalent physician, and most analyses of the costs of delivering primary care services report their findings in the same way, which implicitly assumes that costs are proportional to the number of physicians.↩︎
Pope GC, Burge RT. “Economies of Scale in Physician Practice.” Medical Care Research and Review 53(4):417-440 (1996). Burns LR, Goldsmith JC, Sen A. “Horizontal and Vertical Integration of Physicians: A Tale of Two Tails”, Annual Review of Health Care Management: Revisiting the Evolution of Health Systems Organization Advances in Health Care Management, Vol. 15, pp. 39-117 (2014).↩︎
Basu S et al. “Primary Care Practice Finances in the United States Amid the COVID-19 Pandemic.” Health Affairs 39(9): 1605-1614 (2020).
Patel MS et al. “Estimating the Staffing Infrastructure for a Patient-Centered Medical Home.” The American Journal of Managed Care 19(6): 509-516 (2013).↩︎Kane L. Medscape Physician Compensation Report 2020. Medscape, May 14, 2020.↩︎
U.S. Department of Labor, Bureau of Labor Statistics. May 2019 National Occupational Employment and Wage Estimates, United States.↩︎
The cost of benefits for the physician are assumed to be $30,000 per year, and benefits for other staff are assumed to be equal to 20% of their salary.↩︎
Tinsley R. “The 12-Step Way to Reduce Practice Expenses; Part 1, Staffing Efficiencies.” Family Practice Management March/April 2010, pp. 38-43.
Basu S et al. “Primary Care Practice Finances in the United States Amid the COVID-19 Pandemic.” Health Affairs 39(9): 1605-1614 (2020).↩︎
A physician practice is paid more for seeing a new patient than an established patient, but a visit with a new patient is also expected to last longer. The payments for new patients are generally lower on a per-minute basis, so assuming there are no new patients will slightly overestimate the revenue the practice would receive. However, the vast majority of patient visits in most practices are for established patients, so the impact of this is small. In addition, for most primary care practices, visits rather than procedures represent the majority of revenues, and many practices deliver only a small number of procedures. Procedures frequently require the use of drugs, supplies, or equipment, and the payment for the procedure may or may not cover those additional costs in addition to the time required to perform the procedure, so performing procedures may or may not be profitable for an individual practice.↩︎
Most primary care physicians do not spend significant amounts of time seeing patients in the hospital, in the home, etc. because the additional time required for this prevents them from seeing patients in the office and the payments for services delivered outside the office do not cover the time and costs associated with travel.↩︎
Baron RJ. “What’s Keeping Us So Busy in Primary Care? A Snapshot From One Practice.” The New England Journal of Medicine 362(17):1632-1636 (2010).↩︎
Gottschalk A, Flocke SA. “Time Spent in Face-to-Face Patient Care and Work Outside the Examination Room.” Annals of Family Medicine 3(6): 488-493 (2005).
Chen MA et al. “Patient Care Outside of Office Visits: A Primary Care Physician Time Study.” Journal of General Internal Medicine 26(1): 58-63 (2010).
Doerr E et al. “Between-Visit Workload in Primary Care.” Journal of General Internal Medicine 25(12):1289-92 (2010).↩︎
The physician would need to spend additional time on administrative tasks related to management of the practice. This will likely require several hours per week.↩︎
Some of the slots held open will be filled by patients who do need same-day visits, but because the number of such patients will vary from day to day, the practice will have to have some unfilled slots in order to have sufficient capacity to respond to most requests for same-day visits.↩︎
Office visits for evaluation and management of patients are classified into 5 different levels based on the complexity of the visit. Most primary care visits with established patients are classified as Level 3 or Level 4 visits. Prior to 2021, Level 3 visits with an established patient were assumed to require 15 minutes in face-to-face contact with the patient plus additional time spent after the visit for documentation of what occurred. Level 4 visits were assumed to require 25 minutes of face-to-face contact plus documentation time, and Level 5 visits were assumed to require 40 minutes of face-to-face contact plus follow-up time. Beginning in 2021, the requirements for classifying visits have changed, and the expected visit times are based on the physician’s total time, rather than the face-to-face time with the patient. A visit that requires 20-29 minutes of the physician’s time can be classified as a Level 3 visit, and a visit that requires 30-39 minutes can be classified as a Level 4 visit.↩︎
In 2020, Medicare paid an average of $76.15 for Level 3 Evaluation and Management visits with established patients and $110.43 for Level 4 visits. Assuming that two thirds of the visits would be classified as Level 3 visits and one third would be classified as Level 4 visits, the average payment would be $87. Medicare payments for office visit payments were increased in 2021, but because of the changes in what is required to bill for the different levels of office visit, it is not yet clear how this will affect average payments in the future. Consequently, the Medicare payment amounts in 2020 are used here.↩︎
If the physician sees fewer patients per hour, then most of those visits would likely be classified as Level 3 visits, so Figure 4 assumes the average payment per visit would be lower. If the physician had a significant number of Level 4 visits, then the average payment per visit would be higher, but there would also have to be fewer visits per hour on average. Since the payment per minute for Level 4 visits is lower than for Level 4 visits, total revenues would likely decrease.↩︎
One study found that only 27% of a physician’s time is spent in direct face-to-face time with patients, and that half the time is spent on EHR and desk work related to the visits that occurred during the day or follow-up work from previous visits. Sinsky C et al. “Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties.” Annals of Internal Medicine 165: 753-760 (2016).↩︎
The average number of visits per patient at any given practice will depend on the age of the patients, the number and types of health problems they have, the cost-sharing requirements in their insurance plan, the ease of scheduling visits at the practice, and other factors. Older patients typically visit a primary care practice much more often (an average 4 visits per year or more), and younger patients may visit the practice at most once per year unless they have an acute problem. If one assumes that the hypothetical practice’s patients make an average of 2.3 visits per year, there would need to be 2,500 patients to generate the 5,750 visits shown in Figure 4.↩︎
Murray M, Berwick DM. “Advanced Access: Reducing Waiting and Delays in Primary Care.” JAMA 289(8):1035-1040 (2003).
Altschuler J, Margolius D, Bodenheimer T, Grumbach K. “Estimating a Reasonable Patient Panel Size for Primary Care Physicians With Team-Based Task Delegation.” Annals of Family Medicine, 10(5): 396-400. (2012)↩︎
Davidoff F. “Time.” Annals of Internal Medicine 127(6):483-485 (1997).↩︎
Yarnall KSH et al. “Primary Care: Is There Enough Time for Prevention?” American Journal of Public Health 93(4): 635-641 (2003).↩︎
Østbye T et al. “Is There Time for Management of Patients With Chronic Diseases in Primary Care?” Annals of Family Medicine 3(3): 209-214 (2005).↩︎
Yarnall KSH et al. “Family Physicians as Team Leaders: ’Time” to Share the Care?” Preventing Chronic Disease 6(2), A59. Centers for Disease Control (2009).↩︎
Altschuler J, Margolius D, Bodenheimer T, Grumbach K. “Estimating a Reasonable Patient Panel Size for Primary Care Physicians With Team-Based Task Delegation.” Annals of Family Medicine, 10(5): 396-400 (2012).↩︎
The assumption that more of the patients have chronic conditions does not automatically mean that they would have more acute problems; this is merely an assumption for the purpose of this particular scenario.↩︎
Goroll AH, Berenson RA, Schoenbaum SC, Gardner LB. “Fundamental Reform of Payment for Adult Primary Care: Comprehensive Payment for Comprehensive Care.” Journal of General Internal Medicine 22:410-415 (2007).↩︎
Meyers D et al. “Workforce Configurations to Provide High-Quality Comprehensive Primary Care: A Mixed-Method Exploration of Staffing for Four Types of Primary Care Practices.” Journal of General Internal Medicine 33(10):1774-1779 (2018).↩︎
Chung S, Eaton L, Luft H. “Standardizing Primary Care Physician Panels: Is Age and Sex Good Enough?” The American Journal of Managed Care 18(7) 2012.↩︎
Medicare pays physician practices more if they are located in areas where the costs of operating a practice are significantly higher by adjusting payments using a Geographic Practice Cost Index (GPCI).↩︎
Antonucci J. “Joy Revisited.” Family Practice Management 21(2):36 (2014)↩︎
Ho L, Antonucci J. “The Dissenter’s Viewpoint: There Has to Be a Better Way to Measure a Medical Home.” Annals of Family Medicine 13(3):269-272 (2015).↩︎
Casalino LP, et al. “U.S. Physician Practices Spend More Than $15.4 Billion Annually to Report Quality Measures.” Health Affairs 35(3): 401-406 (2016).↩︎
If it is necessary to charge cost-sharing, an option would be to charge a small copayment for the initial month of chronic condition management services, and then no cost-sharing for the rest of the year. This would be more efficient for both the primary care practice and the patient than billing and collecting small amounts every month (20% coinsurance on the $30 monthly payment would be $6 every month). This approach could help ensure that only patients who have a chronic disease needing proactive care management would enroll for the services, and encourage patients to continue receiving the services once they started.↩︎
Casalino LP. “A Martian’s Prescription for Primary Care: Overhaul the Physician’s Workday.” Health Affairs 29(5):785-790 (2010).↩︎
Eskew PM, Klink K. “Direct Primary Care: Practice Distribution and Cost Across the Nation.” Journal of the American Board of Family Medicine 28(6): 793-801 (2015).↩︎
Ibid↩︎
Kwan LY, Stratton K, Steinwachs DM. Accounting for Social Risk Factors in Medicare Payment. The National Academies Press (2017).↩︎
A patient is classified as having poor control if their HbA1c level was above 9.0% or no HbA1c test result was recorded at all. National Quality Forum. Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%). NQF Measure 0059. Some patients may be managing their diabetes effectively and have an HbA1c lower than 9.0%, but are unable or unwilling to have an HbA1c test performed during the year, or the result was not reported to the primary care practice or health plan that is calculating the measure, so the measure can incorrectly show the level of control for some patients.↩︎
The Core Quality Measures Collaborative was formed by the Centers for Medicare & Medicaid Services (CMS), America’s Health Insurance Plans (AHIP), and the National Quality Forum (NQF).↩︎
National Committee on Quality Assurance. Comprehensive Diabetes Care.↩︎
Lipska KJ, Krumholz HM. “Is Hemoglobin A1C the Right Outcome for Studies of Diabetes?” JAMA 317(10):1017-1018 (2017).↩︎
Miller HD. Measuring and Assigning Accountability for Healthcare Spending. Center for Healthcare Quality and Payment Reform (August 2014).↩︎
If there are 250 Medicare beneficiaries, and average total Medicare spending per beneficiary is $10,000 per year, then Medicare would expect to spend $2.5 million on the 250 beneficiaries during the year. If one of the beneficiaries is treated for lung cancer at a cost of $100,000, total spending would increase to $2.6 million, a 4% increase.↩︎
Center for Medicare and Medicaid Innovation. CPC+ Payment and Attribution Methodologies for Program Year 2021 (December 1, 2020).↩︎
Mathematica. Independent Evaluation of Comprehensive Primary Care Plus (CPC+): Second Annual Report (July 2020).↩︎
CMMI described the 110% factor as a “comprehensiveness supplement” and said it was based on the temporary 10% increase in payments to primary care practices that were required under the Affordable Care Act, not based on an estimate of the cost of providing more comprehensive services.↩︎
In CPC+, the participating practices are also receiving additional revenue from the Care Management Fees.↩︎
Center for Medicare and Medicaid Innovation. Primary Care First: Payment and Attribution Methodologies, Volume 1, Version 2 (December 2020).↩︎
Miller HD. The Problems With ‘Primary Care First’ and How to Fix Them. Center for Healthcare Quality and Payment Reform (2019).↩︎
Miller HD. The Problems With ‘Primary Care First’ and How to Fix Them. Center for Healthcare Quality and Payment Reform (2019).↩︎
Centers for Medicare and Medicaid Services. Medicare Shared Savings Program: Shared Savings and Losses and Assignment Methodology Specifications, Version #8 (August 2020).↩︎
RTI International. Direct Contracting Model Global and Professional Options Financial Operating Policies: Capitation and Advanced Payment Mechanisms (2020)↩︎
For example, the evaluation of the CMS Comprehensive Primary Care (CPC) demonstration, which preceded the CPC+ demonstration, found that 63% of the total patients served by the practices were not “attributed” to the practices and so the practices received only traditional fee-for-service payments for those patients. Mathematica Policy Research, Evaluation of the Comprehensive Primary Care Initiative: Fourth Annual Report (May 2018). Studies of Accountable Care Organizations in the Medicare Shared Savings Program, which uses similar attribution methods, have found that many patients are not attributed to the providers who serve them. See, for example, Ouayogodé MH et al. “Forgotten Patients: ACO Attribution Omits Low-Service Users and the Dying.” American Journal of Managed Care 24(7): e207-e215 (2018)↩︎
Glazier RH et al. “Do Incentive Payments Reward the Wrong Providers? A Study of Primary Care Reform in Ontario, Canada.” Health Affairs 38(4):624-632 (2019).↩︎
Joynt KE, Gawande AA, Orav EJ, Jha AK. “Contribution of Preventable Acute Care Spending to Total Spending for High-Cost Medicare Patients.” JAMA 309(24):2572-2578 (2013).↩︎
Kwan LY, Stratton K, Steinwachs DM. Accounting for Social Risk Factors in Medicare Payment. The National Academies Press (2017).↩︎
Mick EO et al. “Complex Patients Have More Emergency Visits: Don’t Punish the Systems That Serve Them.” Medical Care 59(4):362-367 (2021).↩︎
Johnston KJ, Joynt Maddox KE. “The Role of Social, Cognitive, and Functional Risk Factors in Medicare Spending for Dual and Nondual Enrollees.” Health Affairs 38(4):569-576 (2019).↩︎
Ryan AM. “Will Value-Based Purchasing Increase Disparities in Care?” New England Journal of Medicine 369(26):2472-2474.↩︎
Bernheim S et al. “Influence of Patients’ Socioeconomic Status on Clinical Management Decisions: A Qualitative Study.” Annals of Family Medicine 6(1):53-59 (2008).↩︎
Patient-Centered Primary Care Collaborative. Investing in Primary Care: A State-Level Analysis (July 2019).↩︎
For example, assume that a small Health Plan A pays primary care practices 200% of Medicare rates but has to pay specialists and hospitals 400% of Medicare rates, whereas a larger Health Plan B pays primary care practices 150% of Medicare rates and pays specialists and hospitals only 200% of Medicare rates. Assume that the members of both health plans receive similar numbers of primary care and specialty services, and that if all of the services were paid at standard Medicare rates, the plans would spend an average of $5,000 per year on all services, and $500 (10%) of the spending would go to primary care services. Then Health Plan A would actually spend $1,000 on primary care services (200% of $500) and $18,000 on other services (400% of $4,500), and the percentage it spends on primary care would be 5.3% ($1,000 divided by $19,000). Health Plan B would spend $750 on primary care (150% of $500) and $9,000 on other services (200% of $4,500), and the percentage it spends on primary care would be 7.7% ($750 divided by $9,750). Health Plan B would be spending a higher percentage on primary care, even though its payments for primary care are 25% lower.↩︎
Starfield B, Shi L, Macinko J. “Contribution of Primary Care to Health Systems and Health.” The Milbank Quarterly 83(3):457-502 (2005).↩︎
Goetzel RZ et al. “Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Medical Conditions Affecting U.S. Employers.” Journal of Occupational and Environmental Medicine 46(4):398-412 (2004). Loeppke R et al. “Health and Productivity as a Business Strategy: A Multiemployer Study.” Journal of Occupational and Environmental Medicine 51(4): 411-428 (2009).↩︎
The PTP Column One/Column Two Correct Coding edit file can be downloaded here↩︎
American Medical Association. RVS Update Process. (2022).↩︎
Prior to 2015, Congress required that the update based on the Medicare Economic Index be modified by the “Sustainable Growth Rate” (SGR) formula. This formula threatened large cuts in physician fees every year. In 2015, as part of the Medicare Access and CHIP Reauthorization Act (MACRA), Congress repealed the SGR, but it also eliminated any connection between the Update Factors and inflation.↩︎
American Medical Association. The American Medical Association/Specialty Society RVS Update Committee’s Long History of Improving Payment for Primary Care Services (March 2021).↩︎
Under current law, beginning in 2026, the Update Factor will increase to 0.25% for all physician services, except for services delivered by physicians who participate at a high level in Advanced Alternative Payment Models, who will receive payments based on a different conversion factor calculated using an 0.75% annual Update Factor.↩︎
Section 1848(c)(2)(B)(ii)(II) of the Social Security Act states that increases or decreases in RVUs cannot cause total spending to differ by more than $20 million from what spending would have been in the absence of the RVU changes. Although this requires a reduction in the conversion factor when RVUs are increased, it requires an increase if services are eliminated or the average number of RVUs for existing services decreases.↩︎
American Medical Association. RUC Medical Home Recommendations↩︎
Letter from William L. Rich III to Kerry N. Weems, April 29, 2008, transmitting the recommendations of the American Medical Association/Specialty Society RVS Update Committee’s work relative value recommendations and direct practice expense inputs for the Medicare Medical Home Demonstration project to the Centers for Medicare and Medicaid Services (CMS). Available here↩︎
Thorson D, et al. Adult Acute and Subacute Low Back Pain. Institute for Clinical Systems Improvement (September 2018).↩︎
Short S et al. Diagnosis and Treatment of Respiratory Illness in Children and Adults. Institute for Clinical Systems Improvement (September 2017).↩︎
Swenson PF and Ebell MH. “The Adult Preventive Health Care Schedule.” American Family Physician, May 1, 2016.↩︎
National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. 2020 Focused Updates to the Asthma Management Guidelines. National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (December 2020). National Asthma Education and Prevention Program. Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (August 2007).↩︎
Trangle M et al. Adult Depression in Primary Care. Institute for Clinical Systems Improvement (March 2016).↩︎
American Diabetes Association. “Standards of Medical Care in Diabetes – 2018.” Diabetes Care 41 (Supplement 1) January 2018.↩︎
Garber AJ et al. “Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm.” Endocrine Practice 24(1): 91-120 (2018).↩︎
Fihn SD, Blankenship JC et al. “Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease.” Journal of the American College of Cardiology 64(18): 1929-1949 (2014). Fihn SD, Gardin JM et al. “2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease.” Journal of the American College of Cardiology 60(24): e44-e164 (2012).↩︎
Garber AJ et al. “Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm.” Endocrine Practice 24(1) p. 118.↩︎
Thorson D et al. Adult Acute and Subacute Low Back Pain. Institute for Clinical Systems Improvement (September 2018).↩︎
Fihn SD, Gardin JM et al. “2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease.” Journal of the American College of Cardiology 60(24): e55.↩︎
Sutton RT et al. “An Overview of Clinical Decision Support Systems: Benefits, Risk, and Strategies for Success.” NPJ Digital Medicine 3(17) (2020).↩︎
Centers for Medicare and Medicaid Services. “Medical Loss Requirements Under the Patient Protection and Affordable Care Act.” Federal Register 76(235): 76574 (December 7, 2011).↩︎
Mathematica. Independent Evaluation of Comprehensive Primary Care Plus (CPC+): Second Annual Report (July 2020).↩︎
In contrast, if residents have few choices of health plans, a primary care practice that refuses to contract with non-participating plans could harm both local residents and the practice itself. If the primary care practice is not “in network” for the available health plans, the residents may have to pay higher cost-sharing amounts to receive services and that would make it more difficult for them to receive needed services. If patients have to switch to a primary care practice that does contract with their existing health plan, the primary care practice that wants to deliver high-quality care may not have enough patients to cover its costs even with the higher Patient-Centered Primary Care Payment amounts.↩︎
Network for Regional Healthcare Improvement. Jewish Healthcare Foundation and Pittsburgh Regional Health Initiative (2016).↩︎
Burke T, Cartwright-Smith L, Pereira E, Rosenbaum S. The Antitrust Aspects of Health Information Sharing by Public and Private Health Insurers. George Washington University Department of Health Policy (July 2009).↩︎
Freed M et al. More Than Half of All People on Medicare Do Not Compare Their Coverage Options Annually. Kaiser Family Foundation (October 29, 2020).↩︎
Section 1115A of the Social Security Act created the Center for Medicare and Medicaid Innovation to “test innovative payment and service delivery models to reduce … expenditures … while preserving or enhancing the quality of care.” 42 U.S.C. 1315a.↩︎
The evaluation of the Comprehensive Primary Care demonstration and the first-year evaluation of the CPC+ demonstration both found that there were reductions in total Medicare spending for the patients receiving care from participating practices, but the reductions were not sufficient to offset the additional payments made to the participating primary care practices. Mathematica Policy Research. Evaluation of the Comprehensive Primary Care Initiative: Fourth Annual Report (May 2018).. Mathematica Policy Research. Independent Evaluation of Comprehensive Primary Care Plus (CPC+): First Annual Report (April 2019).↩︎
Actuarial Soundness. 42 CFR §438.4.↩︎
Special Contract Provisions Related to Payment. 42 CFR §438.6.↩︎
Zuckerman S, Skopec L, Aarons J. “Medicaid Physician Fees Remained Substantially Below Fees Paid by Medicare in 2019.” Health Affairs 40(2): 343-348.↩︎
Patient-Centered Primary Care Collaborative. Investing in Primary Care: A State-Level Analysis (July 2019).↩︎
Spending on primary care in 2011-2016 was estimated to range from less than 4% of total Medicaid spending in some states to more than 10% in others. Patient-Centered Primary Care Collaborative. Investing in Primary Care: A State-Level Analysis (July 2019).↩︎
Zuckerman S, Skopec L, Epstein M. Medicaid Physician Fees After the ACA Primary Care Fee Bump. Urban Institute, (March 2017).↩︎
Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032 (April 2019).↩︎
Bodenheimer T, Sinsky C. “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider.” Annals of Family Medicine 12(6): 573-576 (November/December 2014)↩︎
Dalen JE, Ryan KJ, Alpert JS. “Where Have the Generalists Gone? They Became Specialists, Then Subspecialists.” The American Journal of Medicine 130(7):766-768 (July 2017).↩︎